What is bowel cancer?
The most common cancer in Australia (after skin cancer)
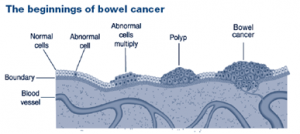
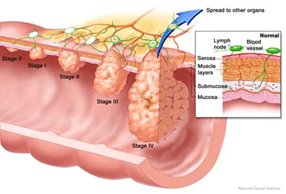
This cancer develops silently over years from uncontrolled, wart-like growths on the inner surface of the large bowel called polyps
Removing pre-cancerous polyps prevents bowel cancer
90 per cent of bowel cancers can be treated successfully, if detected early
Who is at increase risk of getting bowel cancer?
- Before 85 years, the lifetime risk in Australia is:
1 in 10 for men 1 in 15 for women
- Risk increases with age
- Men tend to get it 5-10 years earlier than women
| Approximate risk over the next…. | ||||
| If a person is aged | 5 years | 10 years | 15 years | 20 years |
| 30 | 1 in 7000 | 1 in 2000 | 1 in 700 | 1 in 350 |
| 40 | 1 in 1200 | 1 in 400 | 1 in 200 | 1 in 90 |
| 50 | 1 in 300 | 1 in 100 | 1 in 50 | 1 in 30 |
| 60 | 1 in 100 | 1 in 50 | 1 in 30 | 1 in 20 |
| 70 | 1 in 65 | 1 in 30 | 1 in 20 | 1 in 15 |
| 80 | 1 in 50 | 1 in 25 | ||
Bowel cancer risk is higher for people who have:
- blood passed during a bowel motion
- changes in bowel habits lasting more than two weeks
- prior bowel cancer or polyps
- a family member with bowel cancer or advanced polyps
- colitis for more than 10 years
Do I need bowel cancer screening if I have no symptoms and no family history? YES
- Just by living in Australia, we have the third highest risk of bowel cancer in the world (after Slovenia and New Zealand)
- Bowel cancer is most common in people with no symptoms and no family history
- It is Australia's forgotten, most common, life-threatening but preventable cancer
- If you wait for symptoms, it may be too late to cure
- Earlier detection save lives and improves outcome
- One of the easiest cancers to catch early if screened at a preventable and curable stage (at polyp stage or before symptoms)
- There are several safe, acceptable and effective screening tests available
What screening options do I have after I turn 50? – there is no perfect option
Option 1: Faecal Occult Blood Test every 1-2 years (FOBT stool test) +/- one lifetime colonoscopy at 60-65 years old
- Conveniently done at home, this non-invasive, inexpensive test, detects “invisible” bleeding of early stage “silent” bowel cancer or polyps
- Bowel cancer or polyps may bleed silently for several years. The only way to find this silent bleeding is with a FOBT stool test.
- On a 15 year program, it decreases your chance of dying from bowel cancer 1% per year if you check a FOBT every 2 years and 2% per year if done annually. Namely, it is proven to decrease bowel cancer death by 15% if repeated every 2 years or 30% if repeated annually over 15 years respectively.
- 1 or 2 negative FOBTs is not an “all clear”. Negative test may still have a cancer or polyps. You must stay in the program for over 10 -15 years to be worthwhile
- positive FOBT = bowel cancer only 3-5%. All positive FOBTs need colonoscopy to investigate cause.
Option 2: Colonoscopy every 10 years (starting age: 40 if family history, 50 men, 55 women)
- most accurate, well tolerated and probably the most effective
- proven decrease bowel cancer death by at least 50%
- needs bowel preparation, 2-4 hours in day hospital, sedation
- most costly, and medicare does not covered this option.
- 1 in 500 may have a serious complication
- negative test does not exclude polyps or cancer in 100%.
Option 3: Flexible sigmoidoscopy every 5 years plus FOBT
- This is a common choice in the UK.
- accurate, avoid large volume bowel preparation, no sedation
- only examines left side of bowel where most bowel cancer is found and to decrease risk of missing right-sided lesions do FOBT
- 1 in 15000 may have a serious complication
Option 4: CT- colonography every 5 years
- accurate and easy to perform provided reporting doctor is experienced
- may miss small polyps, needs bowel prep, may be uncomfortable
- radiation dose = 350 Xrays
- need colonoscopy for polyps
- often find irrelevant lesions which bring further worry and require followup testing and scans for month/years
Is bowel screening for me?
- If you are 50 years or over, bowel cancer screening may save your life. Even if 40 years old there can be benefits.
- Australians are being invited to take part in the Government funded National Bowel Cancer screening program using the “FOBT every 2 years” option.
- Over 70% of Australians have probably had some form of bowel cancer screening
- About 70% (even when offered FOBT screening) do not take it up. This may be partly why we have not seen a significant decrease in bowel cancer deaths in Australia since the 1960s.
- Many people who come to a specialist favour colonoscopy every 10 years (or every 5 years if there is a moderate family history). There are also many who choose the less invasive, convenient FOBT stool test at home every year (or two).
- Screening for bowel cancer, when you feel well, have no symptoms and have no family member with bowel cancer, is a preventative health decision.
- Other examples include: asking a doctor for a‘flu shot or to check your blood pressure or sugar level for diabetes, or an annual skin check for skin cancers, or for women, a mammogram for breast cancer or pap smears for cervical cancer or, for men a prostate examination
- Talk your decision over with your doctor. Encourage the people close to you over 50 to do the same. Each option has a set of benefits and risks. None is 100% accurate. Any form of bowel cancer screening may save your life or a loved one and is better than waiting until it is too late.
"Are you over 50?
... then you are at significant risk for bowel cancer.
As Australians we are number 3 in the world rankings after Slovenia and New Zealand"
"Deaths from bowel cancer have not fallen much since the 1960s.
Don’t die from embarrassment. Screening saves lives.”
