Helicobacter pylori gastritis rescue therapy
What is Helicobacter pylori?
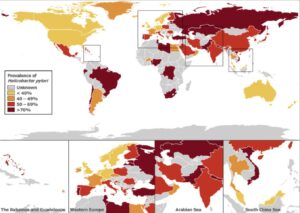
This is an ancient bacteria (germ) able to live in the acidic stomach lining. About 40% of Australians over 60 have it in their stomach lining. Other high risk groups include close family members with peptic ulcer or gastric cancer, migrants or indigenous groups from high-prevalence areas and those from crowded living conditions, institutions or lower socio-economic groups and health professionals with higher exposure to H. pylori positive patients. Most are infected in childhood.
| Decade of birth | Prevalence range (%) |
|---|---|
| Earlier than 1920 | 53.0 |
| 1920s | 20.0–46.0 |
| 1930s | 26.0–37.0 |
| 1940s | 16.7–27.0 |
| 1950s | 11.7–24.0 |
| 1960s | 18.0–18.4 |
| 1970s | 5.0–12.4 |
| 1980s | 4.0–10.0 |
| 1990s | 4.0–8.3 |
It is a harmless coloniser without symptoms in most and a friendly preventer of disease is some. It causes gastritis (an inflamed stomach) in most, gastric or duodenal ulcers in up to 20%, and gastric cancer in up to 2%.
How is it diagnosed?
Urea breath test (UBT)
This test examines your breath for the presence of Helicobacter pylori in the stomach, which can cause gastritis (inflammation of the mucous membranes of the stomach) or ulcers in the stomach and small intestine. The test is a painless and non-invasive procedure that takes about 20 minutes. The test measures carbon dioxide in your expired air, produced as a by-product of the enzyme urease, which Helicobacter pylori produces. You will be asked to swallow a capsule containing radio-labelled urea (14C). Urea is a harmless, naturally occurring substance and the amount of radioactivity involved is approximately the same as half a day’s normal exposure to environmental radioactivity, such as sunlight. An appointment is required for this test. Please contact your local collection centre to arrange an appointment.
Preparation
1. Many medications, particularly some acid-suppressing drugs and antibiotics, can interfere with the test. If possible, and with the agreement of your doctor, the following medications should be ceased prior to your test:
Stop taking all antibiotics and bismuth-containing compounds 4 weeks prior to testing.
Stop taking cytoprotectives (Sucralfate, Ulcyte, Carafate) at least 2 weeks prior to testing.
Stop taking proton pump inhibitors 1 week prior to testing. e.g. omeprazole (Acimax, Losec, HP7 Omperazole Meprazole, Probitor), esomeprazole (Nexium), rabeprazole (Pariet), pantoprazole (Somac). Iansoprazole (Zoton)
Stop taking H2 receptor antagonists 12 hours prior to testing. e.g. Cimetidine Tagamet, Sigmetidine, Magicul Ranitidine Zantac, Rani 2 Famotidine Ausfam, Amfamox, Famohexal, Pecid, Pepcidine Nizatidine Tazac, Tacidine, Nizac
You may continue to take antacids (Dexal, Eno, Gastrogel, Gaviscon, Mucaine, Mylanta, Rennie, Salvital) up to the fasting period.
2. Fast for 6 hours or overnight. This means no food or fluids
but you may clean your teeth. You must not smoke for at
least 2 hours prior to the test.
3. Allow 30–45 minutes to complete the procedure on the
day of specimen collection.
4. Do not have a second UBT within 2 days of your first test.
Please do not discontinue any medication without the
knowledge and agreement of your doctor. from DHM website
How is it treated?
First line: standard triple therapy (PPI+): AMX+CLR 7-14/7, MTZ+CLR 7-14/7
Rescue therapy (PPI+): AMX+LEV 10/7, CBS+TET+MTZ 7-14/7, AMX+RFB 10/7
5th line: Off-label Quadruple therapy: VPZ+AMX+RFB 7/7+ VPZ+CBS+TET 7-10/7
- bactericidals: CLR, MTZ, LEV, RFB
- avoids resistance: AMX, TET, CBS, PPI
- avoid failed combinations
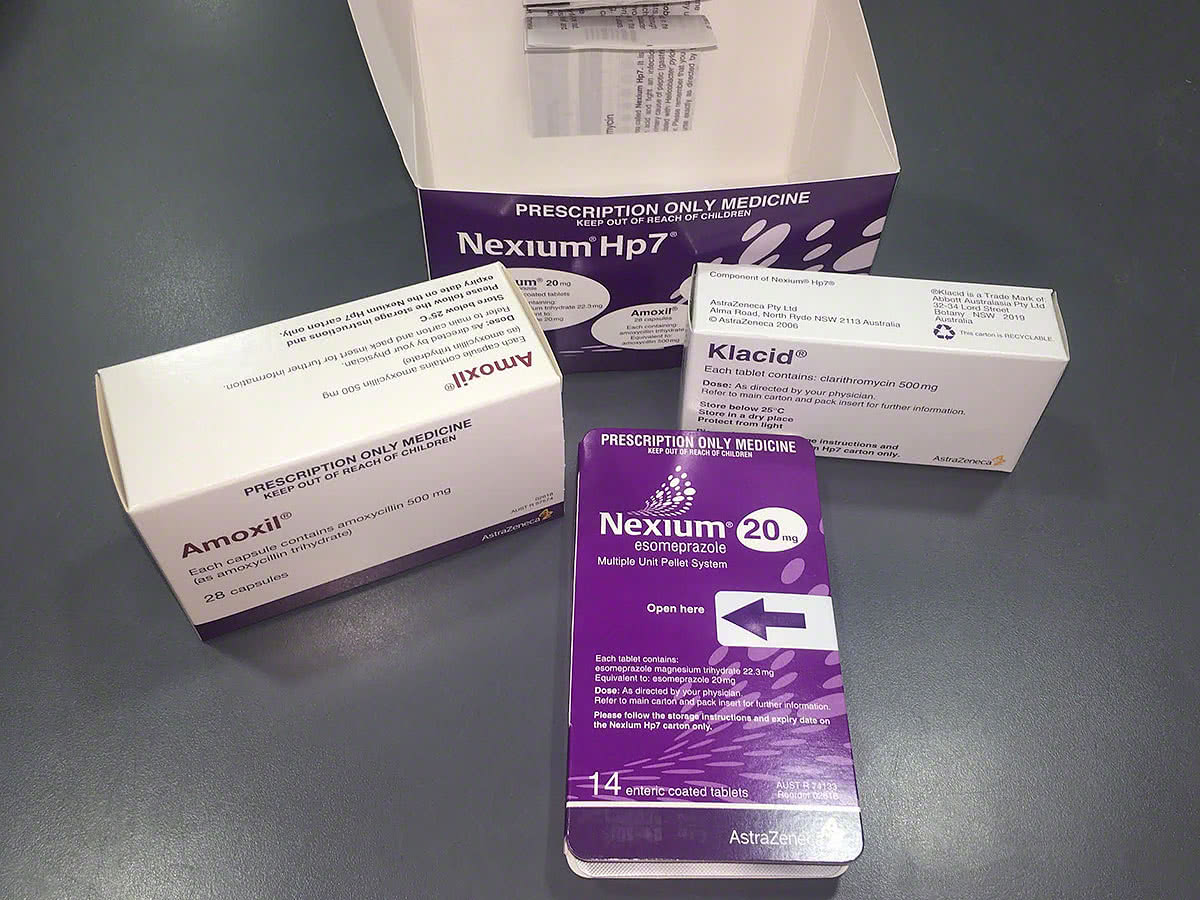
First line treatment is "standard triple therapy". It cures 90% in clinical trials, and somewhat lower rates (>80%) in Australian "real world" settings. Use: 7-14 days (amoxycillin+ clarithromycin + esomeprazole) eg. "Nexium HP7" or, if confirmed true amoxycillin allergy, substitute amoxycillin for metronidazole: clarithromycin (500mg bd - 250mg 14+1 x 2) + metronidazole (400mg bd 21+1) + esomeprazole (40 mg bd).
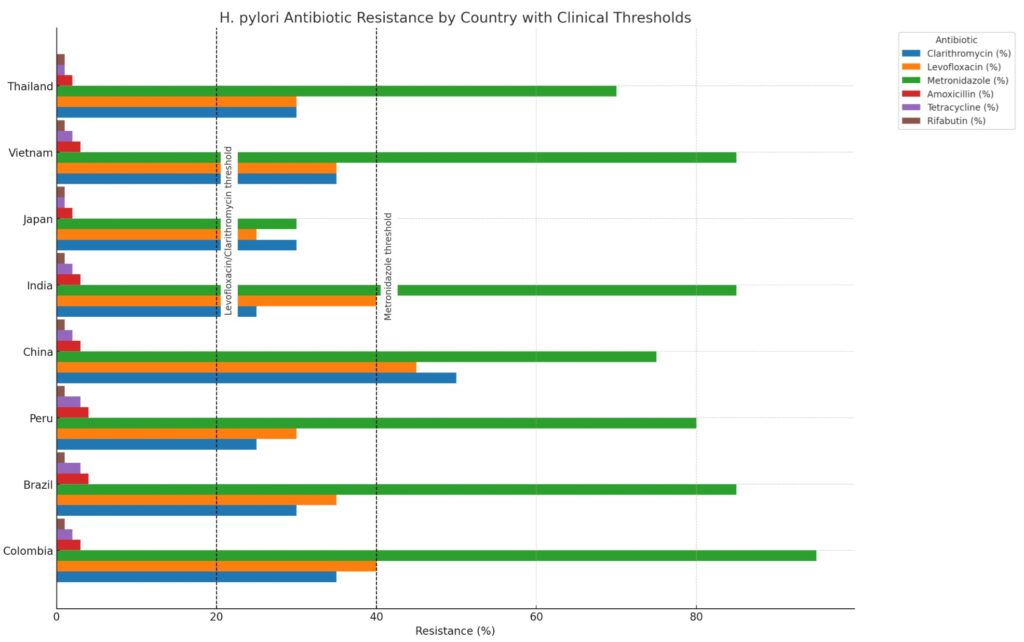
Causes for failure include: non-adherence and resistance (clarithromycin 8-25%, metronidazole 40-50%, amoxycillin rare) depending on country of origin.
Drug interactions (CYP3A4 inhibitor) need consideration with clarithromycin: stop some statins (simv>atorvastatin, not rosuvastatin), colchicine; review dose: QT prolongers/digoxin, anticoagulants (NOAC/warfarin), antiepileptics
Penicillin/amoxycillin allergies rarer than thought: Amoxycillin is a very important part of the treatment for this stubborn infection. Approximately 10% of patients report unable to take penicillin due to allergy. However, up to 90% of these patients do not have a true allergy. Serious allergic reactions to amoxycillin such as anaphylaxis occur in less than 0.05%. If it is not 100% certain you have a true penicillin allergy, or if the history of penicillin reaction is unconfirmed, remote or unconvincing the doctor might send you to an allergist for a blood test and careful skin prick testing.
Rescue therapy (plan A, B, C or D or E) each have 60-80% cure success (depending on resistence patterns):
a) levofloxacin-based 10 day therapy: levofloxacin 500mg+amoxycillin 1g ( 500mg x 40+0 streamline 10402)+ PPI (>+40mg) BD ( esomeprazole 20mg 30+1 streamline 8775) - take 3 medications morning and night for 10 days as directed. Levofloxacin (½ hr before, or if you forget 2 hours after food), Nexium (½ hour before food), amoxycillin (no special directions)
b) quadruple therapy 7-14 days: colloidal bismuth subcitrate 120mg qid +tetracycline 500 mg qid +metronidazole 400mg tds (or qid if resistance)+ high dose PPI (>=40mg) bd*
c) rifabutin-based 10 day therapy: amoxycillin 1g tds + rifabutin 150mg bd + PPI** (>=40mg) bd
d:) amoxycillin 1.5g (iv) tds (375mg x 120 caps) + vonoprazan 20mg tds (30 caps) + bismuth 300mg tds (30 caps), Furazolidone 100mg tds (30 caps), rifabutin 60mg bd d1, 60/120mg d2, 120mg bd d3-10 (60mg 5 caps, 120mg 16 caps) - 10 day Webster pack as directed)***
*Adverse effects are common in up to 50% but less than 5% stop therapy within 5 days due to side effects eg. nausea or vomiting, loose or dark discoloured or black stools or tongue, dry mouth or taste disturbance; clear written instruction maximise adherence. This regimen is often used after failure of levofloxacin-based triple therapy, but may be used beforehand. While taking tetracycline, your skin may be more sensitive to sunlight. Exposure to sunlight, even for brief periods of time, may cause a skin rash, itching, redness or other discoloration of the skin, or a severe sunburn so use careful sun protection measures.
**Since resistance to rifabutin is practically non-existent, and rifabutin therapy is highly effective even in patients with primary resistance to clarithromycin, metronidazole, and levofloxacin, rifabutin usage in an empirical manner may be suggested as “rescue” therapy without culture in those patients in whom these antibiotics have failed. Rifabutin treatment is best left for those experienced in its use. First, this is expensive; second, severe leucopenia and thrombocytopenia can occur (very unusual with short course under 500 mg/day); third, several drug interactions need consideration. Finally, multi-resistant strains of Mycobacterium tuberculosis are on the rise and rifabutin is an important TB drug. So use needs to be limited to avoid further increases in resistance. Rifabutin should be used only as rescue therapy after amoxicillin, clarithromycin, metronidazole, tetracycline, and levofloxacin have failed. Mild to moderate nausea and fatigue occur in <15%
***PPI therapy ideally ≥80 mg/day, amoxycillin ≥3g/day, rifabutin <300mg/day less ADR, furazolidone where metronidazole resistant
Will the triple or quadruple rescue therapy cure my H pylori?
After 30 years of research, there is no ideal H pylori cure without side effects. Even after two "triple therapy" failures (PPI plus amoxycillin plus clarithromycin or metronidazole), H. pylori can still be cured with "quadruple" or levofloxacin-based “rescue” therapy. In "rescue" studies this levofloxacin-regimen (esomeprazole 40mg, amoxicillin 1g and levofloxacin 500mg twice a day for 10 days) worked in over 80%. Traditional "quadruple" therapy has about 70% success.
Consider using different rescue options for immigrants:
Unfortunately, resistance to antibiotics is easily acquired, and in countries with a high consumption of these drugs, the resistance rate is already relatively high. In many regions, clarithromycin and levofloxacin (>20%) or metronidazole (>40%) resistance rates are too high for empiric first line use in H. pylori treatment:
Resistance of H. pylori to antibiotics varies within countries. While resistance patterns are changing rapidly and older studies may no longer be valid, there are some low resistance pockets where standard triple therapy may still work. However, Low-resistance pockets still exist — including rural areas of Southern Taiwan, Northern Thailand, and parts of sub-Saharan Africa and Argentina where antibiotic use is limited. Younger patients (under 20) with no prior exposure to macrolides, particularly in Japan or less urbanised areas, may also have lower resistance rates. Where local data or antibiotic history suggests low resistance, standard triple therapy may still be appropriate. For example here is Regional Indian over the past 10 years
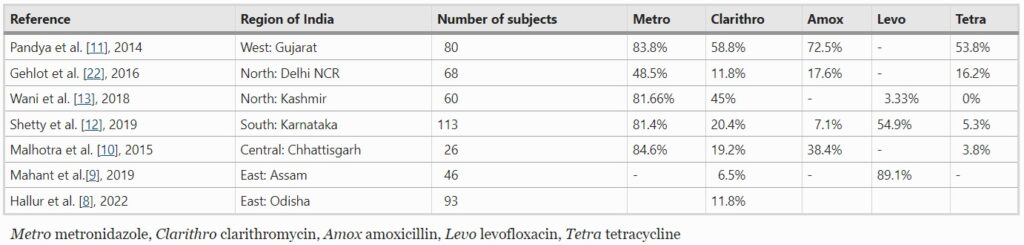 from Dutta, A.K. Choosing optimum regimen for treating Helicobacter pylori infection: Regional data may be the quintessential guide. Indian J Gastroenterol 42, 448–451 (2023)
from Dutta, A.K. Choosing optimum regimen for treating Helicobacter pylori infection: Regional data may be the quintessential guide. Indian J Gastroenterol 42, 448–451 (2023)
What are the possible risks or side effects?
Any decision to treat Helicobacter pylori involves a balance of the risk of not treating against the risk of treating.
Levofloxacin: If you decide to treat with levofloxacin, one study described no side effects in 72% and only 3% had side effects severe enough to require stopping. The most frequent side effects include nausea, headache, diarrhoea, and rashes. There are reported cases of inflamed tendons and tendon rupture and Clostridium difficile diarrhoea.
As with all medications, there is the possibility of unknown risks and late side-effects. However, after more than 15 million prescriptions in the US, the rate seems very low - less than 4 in a million.
Why is levofloxacin, tetracycline, colloid bismuth or rifabutin difficult to find in most pharmacies?
These first three drugs are not registered in Australia. This means the "Therapeutic Goods Administration (TGA) has not evaluated them either for quality, safety and or efficacy” and rifabutin is not approved by the TGA for H pylori infection. In spite of this, levofloxacin does seem simpler to take than quadruple therapy with fewer side effects. Your doctor will need to seek special access from the few special Compounding pharmacies that have supply OR in special cases seek approval from the government TGA (tel: 6232 8111) to use for your condition via a Category B form to Canberra. Levofloxacin cost is about $60-100 depending on health card status and rarely needs a category B form if you apply at the right pharmacy.
Contact your preferred compouding pharmacist or Ramsay pharmacy (T:8425 3911, F: 8425 3910 St Leonards) or Cincotta (T: 98971011, F:88414532) or Customised Compouding (T: 02 8049 9700, 1300 725 868 F: 1300 726 858, info@customisedcompounding.com.au) or Ramdan Pharmacy (T: 9649 4657 Auburn) or Sydney Compounding Chemist (T 9871 7599 Carlingford)
Not less than 4 weeks after your last antibiotic taken and off any PPI mediation (omeprazole Losec, pantoprazole Somac, rabeprazole Pariet, esomeprazole Nexium, lansoprazole Zoton, etc) for 1 week , repeat the urea breath test. Then make an appointment to review the result with your doctor to confirm H pylori cure.
*Dr Samuel has no financial interest in the above Ramsay, Customised Compounding, Ramadan Pharmacy or Cincotta pharmacy. They are pharmacies with expertise in dispensing difficult to attain medicines. Others include: Easy Script Compounding Pharmacy St Marys. You might prefer to shop around as prices vary.