Procedures
Gastrointestinal endoscopies help to diagnose, prevent and treat digestive and liver disorders. They are short day procedures mainly performed under sedation. A small flexible tube camera is passed gently along the digestive tract to examine the inner lining via a magnified image projected on a TV screen. The following are common endoscopic procedures:

Gastroscopy
This procedure is useful to examine the upper digestive tract including mouth, throat, oesophagus, stomach and first part of the small intestine (the duodenum). Once within the upper digestive tract, Dr Samuel may treat several conditions including swallowing difficulties with dilatation or stenting of narrow segments (strictures), thermocoagulation of bleeding vessels or ulcers, banding of dilated variceal vessels, removal of polyps or foreign bodies, Botox injection to segmental spasm or simply biopsy tissue.
Colonoscopy
With new symptoms of changes in bowel habit, rectal bleeding, or lower abdominal pain, this lower digestive tract procedure can be helpful. It is considered the "gold standard" screening test for bowel cancer prevention in higher risk individuals. It is used to remove premalignant tissue (polyps) and to assess other conditions including Crohn's and colitis, diverticular disease and haemorrhoids.
Flexible sigmoidoscopy
This is sometimes called a short colonoscopy. Sigmoidoscopy only examines the last third of the large bowel while colonoscopy examines the whole large bowel. It has the benefit that it may be performed without sedation, that minimal preparation is required and there is even lower risk than a complete colonoscopy. It is often used in assessing for rectal bleeding or lower digestive symptoms when haemorrhoids or other benign disease are suspected.
Double balloon enteroscopy (DBE)
This is an endoscopic technique to examine and treat disorders of the small bowel. These include dilatation of Crohn's strictures, coagulation of difficult to reach bleeding vessels, direct placement through-to-skin of small bowel feeding tubes (direct PEJ), small bowel polypectomy, Peutz-Jegher surveillance programs and retrieval of retained foreign body and "pill cam".
Dr Samuel is one of the few gastroenterologists in New South Wales who performs double balloon enteroscopy (DBE). He performs this procedure at Bankstown hospital. Most patients can have their DBE as an outpatient after a consultation with Dr Samuel. In urgent cases, doctors may contact our endoscopy fellow via the Hospital switchboard (9722 8000). Patients may need to be transferred from another facility without prior consultation. Patients outside metropolitan Sydney, may contact the rooms to arrange a video consultation before the procedure.
Capsule endoscopy ("pill cam")
Also known as "pill-cam" or wireless endoscopy, capsule endoscopy is used mainly to pinpoint bleeding in hidden areas in the small bowel when gastroscopy and colonoscopy fails to find the area. In Australia, we are currently researching and trialing new generation capsules for examination of the gullet and large bowel. This procedure uses a 10 - 27mm capsule, which contains a miniature camera, batteries, light source and transmitter. After swallowing, the capsule travels like a piece of food through the gastrointestinal system to provide over 50,000 high-resolution images of the stomach and small intestine over about 11 hours in total. Recording probes, taped on the abdomen, track the progress of the capsule. The images obtained by the capsule are transmitted to a data-recorder worn in a harness around the waist and later read by the gastroenterologist.
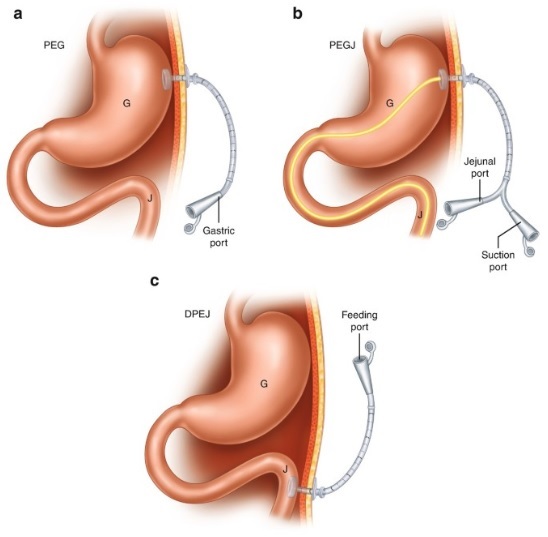
Percutaneous endoscopic gastrostomy (PEG) or jejunostomy (PEJ)
Percutaneous (through the skin) endoscopic (using a endoscopic instrument) gastrostomy (hole directly into the stomach) or direct jejunostomy (hole directly into the upper small bowel) is a safe medical procedure used when swallowing food is inadequate. PEG administration of feeds is a common method of nutritional support for patients in the community. It may be temporary or permanent. Direct PEJ tube is an option when PEG is considered unsuitable. The decision to proceed to a PEG or PEJ tube feeding is often difficult. This is particularly so if the decision is being made on behalf of another person. The key question to answer is “will malnutrition and quality of life be improved with percutaneous feeding?” It is rarely the best option purely to manage functional symptoms such as food intolerance. The decision is made after close discussion with family members, nursing and other allied health professionals including psychologists, medical staff and community contacts.

What about COVID?
In most case, you can proceed with bowel preparation and the procedure if:
- RAT test is negative
- You had a mild COVID illness and are more than 4 weeks from first diagnosis
- You were admitted to ICU with severe COVID and are more than 8 weeks from first diagnosis
- You don't have a reasonable suspicion that you are infectious with COVID
- You are a close contact and COVID negative x 2 (on bowel prep and test day)
- You have mild respiratory symptoms and are COVID PCR negative within 3 days of the test and RAT negative on test day
