Oesophagus and stomach
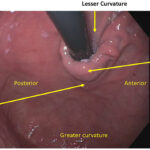
The oesophagus' role is to transport food from the mouth to the stomach. A closed sphincter valve between the oesophagus and stomach relaxes as food approaches allowing the food to pass through it into the stomach. The stomach job is to accept and store this food and then produce stomach acid and other digestive juices to break the food down into smaller, easier to digest fragments. The acid also kills bacteria contained in the swallowed food or saliva. Muscles in the wall of the stomach help to mix thoroughly the food and acid and finally push the partly-digested food down towards the small intestine. Some conditions of the upper digestive tract are included below:
Achalasia and oesophageal motility disorders
In achalasia and other oesophageal motility disorders, the coordinated transportation of food from the mouth to the stomach is disrupted. This leads to symptoms of food regurgitation, chest pain or heartburn, pain when swallowing or the feeling of a permanent lump in the throat. Dietary modifications and several medications can help relieve symptoms, and some disorders can be improved with oesophageal dilatation or botuliinum toxin via endoscopy or surgery.
Barrett’s Oesophagus
Oesophageal and Stomach (Gastric) Cancer
Oesophageal and stomach cancers are malignant tumours found in the tissues of the oesophagus and stomach. They are two separate cancers that can develop in any part of either organ. There are different types of both cancers. They are usually slow growing over many years before any symptoms are felt. Treatment depends on their stage.
Heartburn (Gastro-oesophageal Reflux)
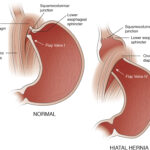
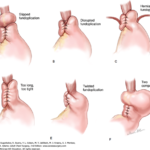
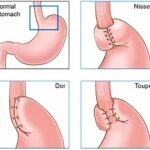
Gastro-oesophageal reflux occurs when the stomach contents, usually acid, backwashes into the oesophagus. Disturbing symptoms include heartburn, acid brash, indigestion, persistent cough, and swallowing problems. It is common. When symptoms interfere with daily life, most can get relief with lifestyle changes and over-the-counter treatments. Some need stronger medications or even surgery.
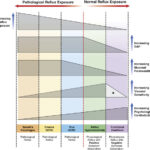
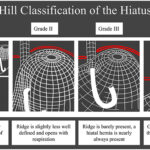
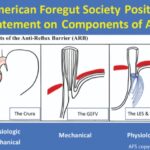
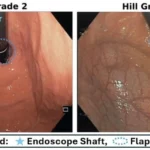
Gastro-oesophageal reflux disease (GORD) is a complex condition resulting from the retrograde flow of gastric contents into the oesophagus. The severity of GORD is influenced by a balance between reflux exposure, epithelial resistance, and visceral sensitivity. Reflux occurs when the anti-reflux barrier, primarily formed by the lower esophageal sphincter (LES) and crural diaphragm, is compromised. This leads to increased reflux events and greater exposure to gastric juice, which can cause damage to the esophageal lining. While acid reflux is a primary factor in esophageal injury, other components of gastric juice, such as bile and pepsin, also contribute to the disease. Complications can arise even with normal reflux levels, particularly when epithelial resistance is low or visceral sensitivity is heightened, so the cause of GORD a dynamic interplay of aggressive and defensive factors.
In addition to the impact of reflux exposure, oesophageal sensitivity plays a key role in the development of symptoms. Some patients with normal reflux exposure experience significant discomfort due to heightened sensitivity, a condition known as reflux hypersensitivity. Factors such as stress, anxiety, and psychosocial comorbidities can exacerbate symptom severity and affect response to treatment. Research into the mechanisms of GORD continues to evolve, with new insights into the roles of mucosal barrier function, sensory nerve sensitivity, and central nervous system processing. Advances in understanding these processes may lead to more effective, personalised treatment strategies for GORD patients in the future.
Eosinophilic oesophagitis (EoE)
EoE is an increasingly recognised oesophageal disorder where the oesophagus is inflamed with an increased number of high specialised immune cells called eosinophils. It commonly causes difficulties swallowing solid food including food impaction, and non-swallowing associated chest pain. It may occur at any age with a peak in 30-5o year old males. Food allergy, hay fever, asthma and eczema are common. Treatment is helpful with topical anti-inflammatories called glucocorticoids, acid suppression, food elimination diets and endoscopic dilatation of narrowings where medications is unhelpful. Monitoring is mainly done with biopsy after 6-12 weeks of treatment as symptoms correlate poorly with the severity of inflammation. There is no association or link to cancer. See below links for:
Mistakes in EO and how to avoid them
Gastroparesis
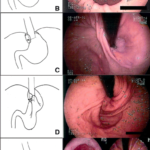
Gastroparesis is a disorder of the nerves or muscles of upper digestive tract where the stomach cannot empty itself of food and liquids in the normal way. Symptoms include feeling sick, nauseated, full or bloated when eating, vomiting, pain in the upper abdomen and weight loss. The diagnosis is not always easy and tests to confirm the diagnosis may include Xrays, gastroscopy, nuclear medicine tests of gut motility and function and on occasions a test called antroduodenal manometry. The cause is not found in nearly half of cases. Other causes include diabetes (nearly 25%), postviral/infectious states, connective tissue or autoimmune disorders, prior stomach surgery, poor blood circulation to the upper digestive tract (so called ischaemia) and medications. Gastroparesis patients show diverse changes in function of the upper digestive tract including abnormal muscle tone in the upper stomach (abnormal fundic tone), poor coordination of muscle contractions within the stomach and then between stomach and duodenum (gastric dysrhythmias and antroduodenal dyscoordination, impair duodenal feedback), decrease strength of the muscle waves which emptying the stomach (weak antral pump). Treatments including diet changes, medications to accelerate gastric emptying or against nausea and vomiting, pyloric botox or dilation. In some tough cases, Xray or endoscopic procedures including small bowel feeding tubes via the nose or through the abdominal skin. As these tubes passing via the stomach into the small bowel may be disrupted by vomiting. other novel techniques may be needed if nutrition is suffering. Since 2009, Dr Samuel has been using a novel minimally invasive double ballooon enteroscopy assisted technique to bypass the stomach and place feeding jejunal tubes directly through the skin (direct PEJ). In other cases patients are referred for surgical procedures including stomach pacemakers to provide relief of symptoms and help with nutrition. With a tailor approach symptoms, nutrition and quality of life can be significantly improved.
Peptic Ulcers and Helicobacter pylori
Swallowing Disorders
With careful assessment, most swallowing disorders can be clarified and treated. Often speech therapy, lifestyle change or medication is enough. Occasionally oesophageal dilatation, "Botox" injection, surgery or percutaneous feeding gastroscopy is required.[/vc_column_text][/vc_column][/vc_row]