What is a double balloon enteroscopy (DBE)?
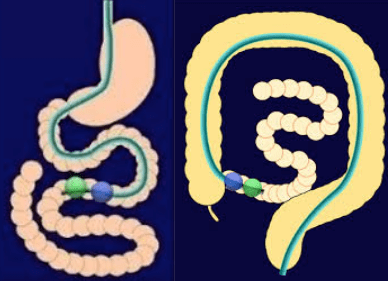
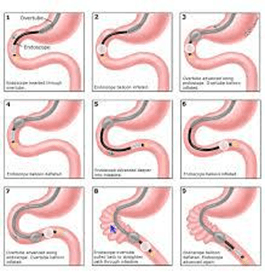
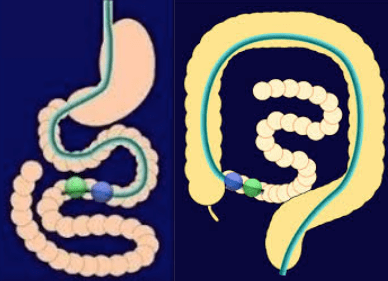
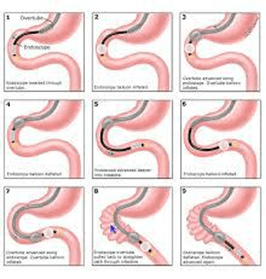
This is a procedure to examine the complete lining of the small intestine- the middle part of the digestive tract. The DBE system can get to areas beyond the reach of conventional gastroscopy and colonoscopy. It includes a long flexible tube camera called an enteroscope and overtube. Both are fitted with a balloon at the end. Under deep sedation, the DBE system is passed either anterograde (via the mouth) or retrograde (via the rectum) and gently moved along the bowel (inflating then deflating with air) to access deep into the small intestine. A magnified image of the small bowel's inner surface is projected on a TV screen. It can be used to diagnose or treat small bowel diseases and to place percutaneous enterostomy tubes. The test can take over an hour. Plan 2 - 4 hours for waiting, preparation and recovery and bring a good book. Depending on the procedure you may be admitted for observation.
Who is responsible?
Dr Douglas Samuel will perform the test with another doctor assisting. An experienced team lead by an anaesthetist will sedate you and ensure your comfort and safety. Dr Samuel is one of three senior gastroenterology colleagues, which include Dr Ahmad Alrubaie and Dr Chris Meredith, who have been providing the DBE service for over 10 years at the Bankstown Hospital endoscopy unit. In urgent cases, with your consent, one of his two colleagues may perform the test.

What happens before the test?
On booking, you will be given an admission form with an endoscopy session (eg. Thursday afternoon 5 September 1-6pm) at Bankstown Lidcombe hospital endoscopy unit. Occasionally, we may call you to change it. Dr Samuel's team will contact you a few days before and after your test to help prepare for the day and provide you with extra support after of your procedure. To change or cancel your booking, please call my rooms as soon as possible, to allow for others on the waiting list.
Bankstown Lidcombe Hospital (BLH)
Please complete pages 13-15 of the admission form and deliver to BLH at least 7 working days prior to your test. If you are unable to deliver the original in this time, ensure a copy is sent to our rooms and bring the original on the day of your test. You need to call BLH staff on 9722 8453 to confirm your admission time 3 working days before your test. Please contact BLH billing department for any hospital billing inquires if you are not medicare eligible.
Can I take my current medications?
Most medications (including aspirin) can be continued. Be sure to tell our staff i) your drug reactions or allergies, ii) if you need antibiotics for dental procedures and iii) if, in the past 3 months, you have taken: aspirin, blood thinners (eg. warfarin, clopidogrel, rivaroxaban), insulin or prednisone. If you are on the “pill,” use another contraceptive for 2 weeks after your procedure. Stop anti-diarrhoea or iron pills five days before. If you use steroid puffers for asthma, use them at usual or increased dose for 5 days before the procedure. If you take diabetes pills or insulin - then on test day, these must not be taken unless instructed - on the day before the test, take half the usual insulin and be careful with “hypos”. Bring an up-to-date list of all your medicines to hospital.
What if something abnormal is found?
If an area needs further testing, you will have a biopsy (a rice grain-sized sample of colon lining). Bleeding lesions may be controlled with special techniques. If you have polyps (benign growths on the bowel lining) these will be removed called polypectomy. Biopsy and polyp removal is not painful. Other treatments include dilatation of narrowings called strictures or argon plasma coagulation of bleeding lesions.
What are the risks?
Before your procedure, you will have an opportunity to ask questions particularly about the benefits and risks of your DBE and have these answered in a way that you understand. DBE is very safe. When you take bowel cleansing laxatives for a retrograde (via rectum) study, then nausea and bloating is common and rarely lasts long. Unusual colon anatomy or poor bowel cleansing sometimes make completed retrograde DBE impossible. In this case, your doctor may order a repeat or another test or may feel the limited examination is enough. Even with the best techniques, bleeding lesions, polyps and tumours can be hidden from view and missed. The bowel wall may be unusually fragile and puncture or bleed. Bleeding after polyp removal is usually minor and stops on its own. Complications needing urgent surgery are rare (1 in 1000). Other uncommon problems include sedative or bowel preparation reactions, infections or worsening of existing heart or lung disease. Although complications are uncommon, it is important to recognise them early. Contact your doctor or hospital if you notice severe abdominal pain, dizziness, fever, chills, rectal bleeding (more than 1/2 a cup) or severe shortness of breath. Bleeding can occur up to 14 days after a polyp removal.

Are there alternatives?
DBE is considered the best test for same time diagnosis and treatment for small bowel diseases. CT scan, MRI and capsule endoscopy may have a role. Discuss the alternatives with your doctor to help choose.
Three steps for bowel cleansing: what do I need to do?
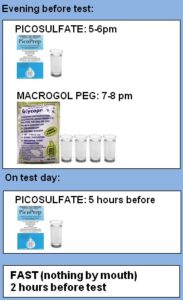
This is only need if you have been scheduled for a retrograde study (via the anus). It involves the same preparation as a colonoscopy including a diet change and some laxatives. This is usually the most troublesome part of your procedure. See 10 tips for surviving the bowel prep below. If possible for 48 to 24 hours prior, take no seeds, nuts and raw vegetables, skins or whole grains including bread with seeds. For 24 hours to 2 hours prior, drink only clear fluids and take no solid food. Please buy Prepkit C (no prescription needed) from your local pharmacy. You will find 3 sachets of laxative salts. For a procedure after 10:00am, take two sachets the afternoon/night before and, one on the morning 5 hours before the test. If your colonoscopy is before 10am then take the third sachet at 9pm. Some occasionally will need an enema on test day. If bowel cleansing is inadequate, you may be cancelled or rescheduled, as abnormalities including bowel cancer may be missed.
48-24 Hours (two days) before colonoscopy
LESS FIBRE and ROUGHAGE
Limit seeds, nuts, uncooked vegetables, skins and whole grains from 48 hours
24-2 hours (one day) before colonoscopy
CLEAR FLUIDS ONLY
Water, clear fruit juices (apple, pear, white grape), coconut water, jelly, skim milk, Bonox, black tea/coffee, honey, carbonated beverages, clear cordials (lemon/lime), Ensure ® (<3 cans), sports drinks (eg.Gatorade ®), popsicles, sorbet/gelati. Clear broth/bouillon (STRAIN chicken/ beef/vegetable noodle soups). Hard/gelatine sweets (eg. barley sugars, lollipops, gummy bears), small volume of clear alcohol (light beer, white wine, vodka, gin, whiskey etc)
Take care to avoid dehydration.
Drink 2-3 glasses or serves of clear fluids throughout the day at: breakfast, morning tea, lunch, afternoon tea, dinner and evening (and test morning up to two hours prior)
IT’S CLEAR, IF YOU CAN READ NEWSPAPER THROUGH IT
No solid food, full cream milk nor red/purple food colouring
BOWEL CLEANSING ORAL SALT FLUSH with “Prepkit-C”: take two sachets the evening before and one on test day
Buy Prepkit C (3 sachets) well in advance from a local pharmacy
No prescription required
"PICOPREP" (x2): add (sachet A or C) to ONE 250mL glass, drink over 30 minutes
"GLYCOPREP C" (x1): add (sachet B) to FOUR 250mL glasses (or 1L jug). Drink 1 glass every 15 mins. If you start to feel nauseous, slow down
Expect diarrhoea (30 mins to 4 hours) after drinking laxative sachet
FOR TEST AFTER 10AM*
FOR TEST BEFORE 10AM*
* FOR TEST BEFORE 10AM
Your options for the third (Picoprep) sachet depend on when you like to sleep. They are to take it:
- at 9pm (ie take each at 5pm, 7pm, 9pm) - most common
- at 3pm (ie take each at 3pm, 5pm, 7pm)
- 5 hours before (eg. for a 10am test, after setting your alarm! take each at 5pm, 7pm and the next day at 5am )
TEN TIPS FOR SURVIVING THE BOWEL PREP
- Prepare laxative mixtures in advance and chill well
- If you feel nauseous, slow down
- Add lemon juice, ginger ale or lime cordial (but only if you never want to drink that beverage again in your life ! )
- Chill glass, drink with a straw and rinse mouth after drinking
- Suck on sweets
- Stock up on peppermint tea, lemonade iceblocks and ginger ale beforehand
- Apply Vaseline or Zinc oxide to your anal area in advance and use baby wipes instead of toilet paper
- Ensure safe, well-lit bathroom access, particularly at night, to prevent falls or accidents
- Don't be afraid to bring some entertainment to the bathroom, you'll be there a while
- Drink clear fluids right up to 2 hours before your test
If you feel you'd be more comfortable to be admitted the night before your colonoscopy for extra nursing care, please let our rooms know.
SPECIAL GROUPS
These conditions may need special instructions for bowel preparation
- diabetes
- severe constipation
- prior inadequate bowel preparation
- severe kidney disease
- liver cirrhosis
- heart failure
- colonoscopy before 10am
What if something abnormal is found?
If an area needs further testing, you will have a biopsy (a rice grain-sized sample of colon lining). Bleeding problems may be controlled with special techniques. Usually, if you have polyps (benign growths on the colon lining) these will be removed called polypectomy. Polypectomy is an important way to prevent bowel cancer. Biopsy and polyp removal is not painful. If haemorrhoid bleeding or discomfort are a significant problem, ask about treating these while sedated with non-surgical techniques including rubber band ligation or infrared coagulation. These haemorrhoid treatments, while associated with less pain and risks than haemorrhoid surgery, may cause manageable short term pain or discomfort for a few hours to days.
What happens after double balloon enteroscopy?
On waking, you may feel wind pain, bloating and pass air introduced during the test. You may have discomfort at the vein access site on your arm. Even if you feel alert, your judgement, memory and reflexes will be impaired for the rest of the day. Your doctor will see you after the test and give you your results with a written report. It is common to have no memory of the test or discussion. Someone familiar must drive you home and stay with you after the procedure. Our hospital policy does not allow taxi services. Do not drive your car, sign legal papers or send important emails, drink alcohol or operate machinery until the next day. A report with biopsy results will be sent to your referring doctor after about a week. It is important that you ring the rooms to make and keep a follow up appointment with your specialist to discuss the results.