Low FODMAP diet
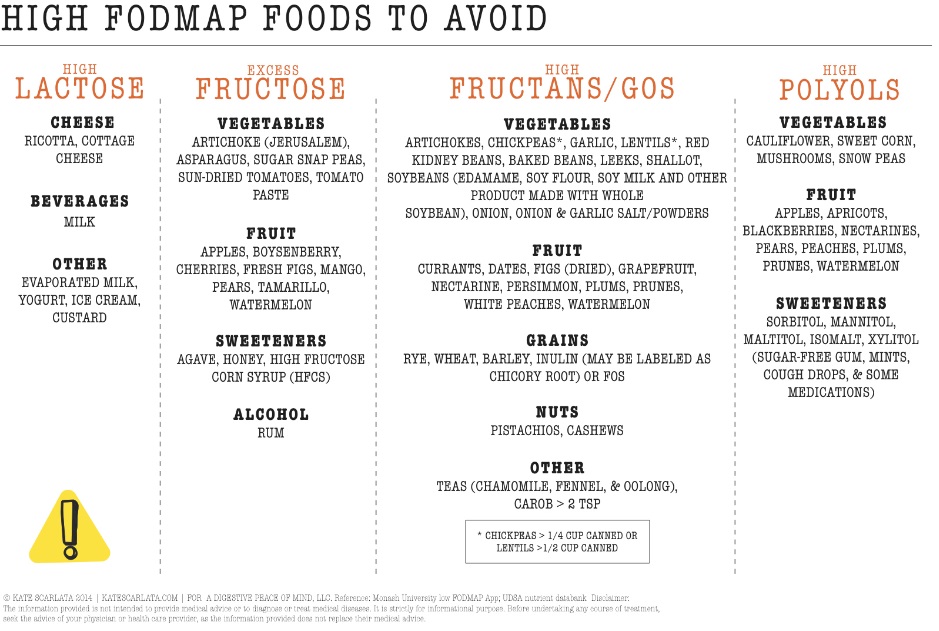
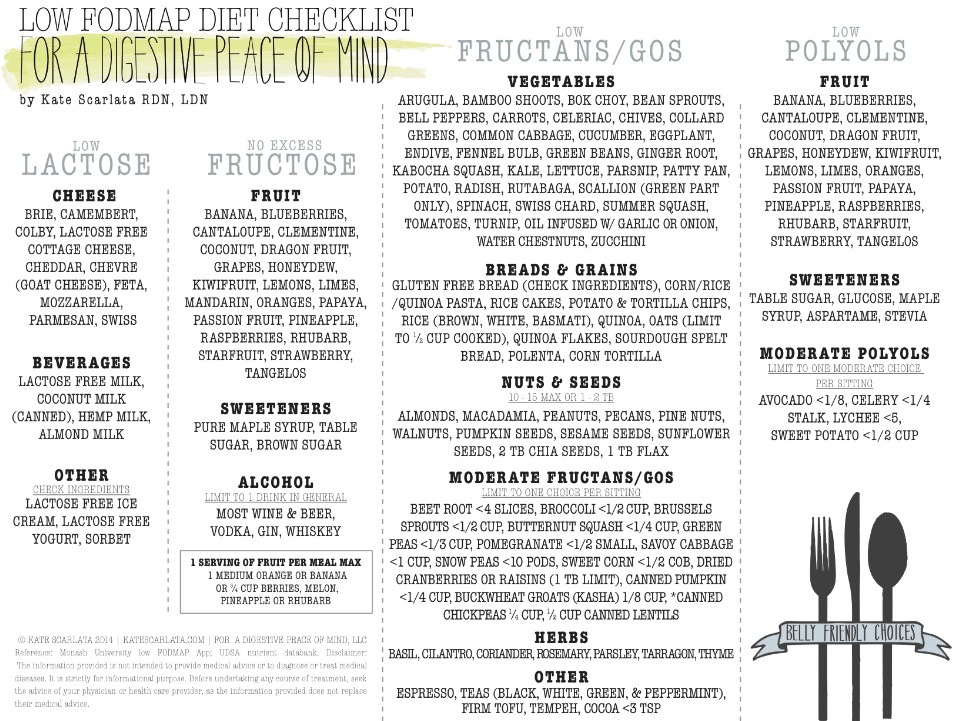
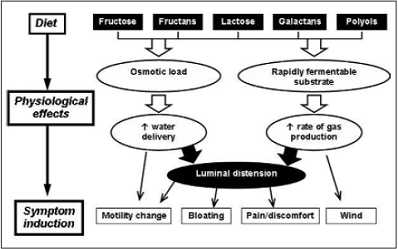
FODMAP is an acronym for a group of short chained carbohydrates, common in a Western diet, (Fermentable, Oligo- Di- and Mono-sacharides And Polyols) which can be the hardest of all food sugars to digest. The low FODMAP diet is gaining attention in functional and lifestyle medicine to help those seeking control of distressing gut symptoms. They are in:
- dairy (milk, cheese, ice cream, yoghurt)
- wheat (bread, pasta, pastries, cakes, and biscuits)
- some fruit
- onions and garlic
- cabbage and cauliflower
- legumes (beans, soy, and lentils)
- low-calorie sugar-free products and confectionary.
There are health benefits and drawbacks to a diet rich in the foods that contain FODMAPs type sugars. What you find below has been written to help those choosing to navigate this diet change.
Despite "carbs" (or carbohydrates) being the new food enemy in our popular press, they are the main source of calories in a healthy diet and are the primary fuel for the brain and muscles. Foods high in FODMAPs are usually rich in health-promoting nutrients including fibre, starches, complex carbohydrates, phytochemicals, vitamins, minerals, and prebiotics for a healthy gut microbial diversity and bowel regularity. For all but a few, they need to be IN (and NOT OUT of) of the healthy diet.
If too many FODMAPs are eaten in one sitting, the digestion may get overloaded. A fast gut transit, seen with some forms of functional gut disorders or exercising straight after eating, may make it worse still. Undigested FODMAPs cause gut fluid retention leading to loose or frequent bowel motions; or they get fermented by healthy gut bacteria causing intestinal gas and bloating. For most, this change in bowel habit or wind for a few days is a normal part of life and not distressing. However, for some, it means trouble. If you have a sensitive or disordered bowel function or transit, then temporarily limiting FODMAPs in your diet, can stop distressing gut symptoms including nausea, fullness, belching, bloating and wind, gurgling, cramping pains, diarrhoea, constipation, urgency and flatulence. A very rare few need to make this diet a permanent life long change.
"I had several distressing months of nausea, abdominal gurgling, bloating, cramping abdominal pains and loose urgent motions. After multiple tests, I was told I had a function gut disturbance that some might call the irritable bowel syndrome. The doctor felt some plant sugars or carbohydrates in my diet called FODMAPs might be the problem. I was having these daily in milk, chewing gum and sweets, orange juice, fruits, vegetables and low-cal soft drinks. I went on a “low FODMAP diet” for 3 weeks, stopped a magnesium supplements and my diarrhea and cramps got much better. I slowly restarted the excluded foods and found I could tolerate most food in lower amounts without problems. I feel the best I have in years.” Julie 32 yo flight attendant
Before starting a low FODMAP diet
1. Customise your diet. Everybody's FODMAP tolerance is different. Take time to work through elimination and challenge phases. A dietitian may help. It depends on:
- FODMAP type and preparation
- FODMAP dose
- your own gut’s sensitivity, enzyme levels and function
A small amount of dried fruit in a very sensitive gut may cause no symptoms. Large quantities of cabbage, beans and onions in the most “iron stomach” will cause gas and change in bowel habit. Working out the diet balance which fits your lifestyle can be overwhelming. You may prefer to see a dietitian. This is Medicare rebatable in Australia if your GP refers you.
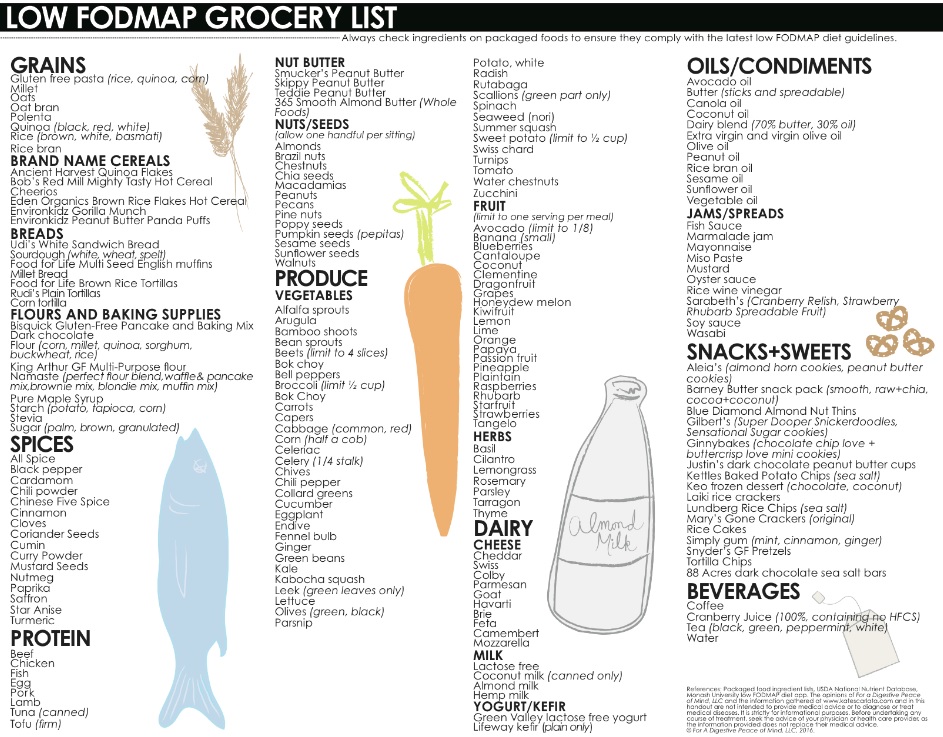
2. Treat your constipation and slow gut transit (which may not be obvious to you). Constipation is a common cause of food intolerances; treating it can make you better able to tolerate high FODMAP foods. Also cutting back on FODMAPs (in wheat, rye, barley and legumes) make it hard to get to the daily Australian fibre recommendation to consume 25-30g. This can worsen constipation. So getting this right is critical, including:
- five serves of low FODMAP vegetables (consider white potato with skin, 1/4 cup canned chickpeas (drained and rinsed) or 1/2 cup canned lentils (drained an rinsed)
- two serves of low FODMAP fruit per day (snack on banana, an orange, kiwi fruit; add blueberries, strawberries stewed fruit, or frozen berries on to cereal or yoghurt)
- multigrain gluten-free or spelt bread (the darker and grainer usually means more fibre)
- brown rice, quinoa, corn or oats
- add low FODMAP seeds and nuts to your diet. Snack on small amounts (1-2 tablespoons) of almonds, brazil nuts, pecans, walnuts or make your own peanut or other nut butters, add very small servings (1 tablespoon) of chia seeds, oat bran/oatmeal, LSA, pumpkin seeds or rice bran to a smoothie or cereal
- consider less fermenting fibre supplements like psyllium ("Metamucil"), linseeds, oats, sterculia (“Normafibe”) and methylcellulose. Fibre supplements that contain highly fermentable wheat bran, fructo-oligosaccharides (FOS), inulin and galacto-oligosaccharides (GOS) tend to promote colonic gas exacerbating IBS. There is little good studies on wheat dextran ("Benefiber"). However this, along with partially hydrolysed guar gum ("Sunfiber"), may be worth trialing. When starting a fibre supplement, begin with a small dose and slowly increase this over several days to the recommended dose.
- don't forget protein with meat, fish, tofu
- 8 glasses of non-caffeinated, alcohol-free fluid a day, and,
- regular sleep discipline
- a physical activity or exercise that works for you.
3. Keep up on calcium rich foods when lactose free, rather than use a supplement. Schedule daily snacks and meals with:
- lactose free cow's milk, lactose free yoghurt, hard cheeses
- calcium-fortified soy milk or other plant milks (a good nutritional benchmark to look for is 120mg of calcium per 100ml serve), calcium-set tofu
- almonds, Brazil nuts, sesame, chia seeds
- canned tuna, sardines or salmon with bones
- kale, bok choy, okra, rocket
4. Watch portion control and follow the age-old "everything in moderation” approach.
A Japanese proverb has it, “eight parts of a full stomach sustain the man; the other two sustain the doctor". The long-term safety of daily FODMAP restriction has not been formally reported. For example, oligosaccharides (the O in FODMAPs) may have prebiotic benefits in bowel cancer prevention. The low FODMAP diet is not to be used as a fad exclusion diet. It is a strategy to explore of which food to eat less when you have digestive symptoms. Do not rigidly exclude any FODMAPs life long until you have a medically confirmed condition such as coeliac disease or a true food allergy. Excluding food from your diet in this way may effect your nutrition, limiting the many health benefits of food diversity and lead to unnecessary worsening of food intolerance when you reintroduce the food at a later date. Also, as you learn to calm your digestive system and look to better eating habits, consider having three smaller meals per day with two snacks in between; consider slowing down while you eat, enjoying meals without screen distractions (mobile phones, TV etc.); try taking in some long, slow breaths before your meal can also help calm the nerves and make you less likely to overeat and try following the Confucian teaching to stop eating when you are 80% full.
5. Choose snacks from Nature rather than from "Boxes, Plastic bags or Cans":
- popcorn or rice cakes
- banana and natural peanut or other nut butter, an orange, handful of almonds
- baby carrots and cucumber with tahini or dilly dip (blend ½ cup lactose free cottage cheese with fresh chopped dill, parsley, sea salt, pepper in blender until creamy)
- "hard cheese" sticks
6. It's not only dietary FODMAPs that make digestive symptoms worse. You might also improve windy symptoms and discomfort if you try to decrease:
- high-fat foods (including fried, fast food, processed meats)
- beer and other alcohol
- red meat, sausage
- egg yolks
7. Try these helpful resources:
8. Be careful the over-the-counters and supplements, lactose free drinks or snacks you take are not not high in other FODMAPs (eg. ):
- tablets or probiotics with FOS or inulin
- gluten or "sugar" free foods with ingredients added such as: agave syrup, honey, chicory root extract, pear or apple concentrate
- granola bars with dates, honey or chicory root extract
- whole soybeans such as edamame, crushed soybeans or soybean flour (rather than soy protein extract) or other bean flours
- for athletes wanting low FODMAP protein powders such as rice, egg, sacha inchi protein, and whey protein isolate powders, check for other high FODMAP ingredients. Avoid whey protein concentrate and hydrolyzed whey protein (unless it says lactose free).
9. The low FODMAP diet may not help 30% with functional gut disorders. If it doesn't improve distressing "windy" symptoms, bloating, diarrhoea or constipation, make sure your doctor has rule out, the many common reasons. With different approaches, these can be successfully treated and include:
- Coeliac disease, inflammatory bowel disease like Crohn's, or parasitic infections
- bile salt diarrhoea and small bowel bacterial overgrowth syndrome (also referred to as BAD and SIBO)
- endometriosis, pelvic inflammatory disease
- dyssynergic defecation, pelvic floor dysfunction or bowel obstruction
- acute or chronic stress, sleep disorders, anxiety or depression
- "Over-nutrition" - overdoing high GI or fatty/oily foods, alcohol or caffeine
- mast cell disorders or food allergy
- natural food chemical or food additive sensitivity (eg. salicyclates, amines, glutamates) or non-coeliac gluten intolerance
10. Don't ignore other parts of your physical and psychological wellbeing while you look at food. A healthy diet is only one important goal in keeping a healthy digestive system. Find a friend or professional to talk to about the stresses in your life. Need a little external help to keep to your health commitments, you might request that they hold you to account. Important health goals beyond diet that may help you cope better with the unpredictability of gut symptoms include:
- managing your thoughts, mood and worries
- regulating life’s rhythms particularly your sleep/wake cycle
- physical activity
- balancing work and play
- seeking meaning and spirituality
- connecting with others
- accepting change and imperfections
For self-help, try the below strategies. If strategy one doesn’t work, then try strategy two or visa versa:
Trialling the Low FODMAP diet
Strategy 1: four 2 week diets – diet A alone first, then: diet B(low lactose),C(low wheat/onions/garlic) and/or D(low fructose) with diet A separated by at least a week. Keep a diary of symptoms, stressors and life events, your cycles (sleep times and your menstrual cycle if female) and food.
Strategy 2: try a low FODMAP diet (diet A-D) for 2-6 weeks. Then, after at least 2 weeks, introduce “unfavourable food” every fourth day. For example, start with fructose. As fructose can take up to 3 days to pass through the digestive tract, try a small amount of high fructose “unfavourable food” every four days. If this is OK, try having it more frequently, then build up the quantity. Cut back again if symptoms recur.
Group A: the "big wind makers" : Brassicas, Legumes and Polyols
decrease raffinose and galacto-oligosaccharides: Cruciferous group - Cabbage, Brussel sprouts, Cauliflower, Broccoli, Asparagus, Legumes – chickpeas, lentils, red kidney beans, baked beans, soy.
Try alternatives: carrot, potato, zucchini, lettuce, squash, green beans, pumpkin, parsnip, corn, eggplant, or maximum one handful per sitting of nuts (almonds, macadamias, peanuts, pine nuts, pecans ) or seeds (sunflower, sesame, pumpkin);
and,
decrease sorbitol and other polyols: Apricots, Peaches, prunes, Nectarines, Cherries, Plums, apples, Pears, artificially "sugar-free" sweetened gums, toothpaste, mints, lollies, cough medicine, artificial sweeteners ending in ‘ol’: sorbitol, mannitol, xylitol, isomalt, polyglucitol, lactitol, erythritol, maltitol
Try alternatives: maple or golden syrup instead of honey
While you may choose to avoid these in the short term, in the longer term, cruciferous vegetables, beans, lentils and peas are important part of your recommended five daily portions of fruit and vegetables. These Group A vegetables are a cheap, low-fat source of fibre, phytochemicals, vitamins and minerals. In the case of cruciferous vegetables they may have extra cancer prevention benefits (such as potential cancer preventing glucosinolates). Legumes are also a rich source of protein for vegan and meat eater alike. However, no-one can digest these well. We humans lack the alpha-galactosidase enzyme in our small intestine that is required to break down raffinose, so it passes through our digestive tract completely undigested. Once in the colon, the bacteria there thrive on it and ferment it into large volumes of hydrogen, methane and other gases.
There are a few tricks. You can reduce the amount of raffinose in dried beans by soaking them overnight in water with a tablespoon of vinegar. Drain them before you cook them in fresh water. A capsule of Bean-zyme taken with high raffinose foods, like beans and peas may give enough of the digestive enzymes you need to break down the oligosaccharides before they can cause bloating and gas. Some have noted that adding natural anti-gas fennel seeds to a recipe with legumes can also help. Others find slowly building up the dose over time allows the gut microbiota to adjust.
What is interesting with peas, beans and other legumes is that eaten on their own they often cause large volumes of intestinal gas, but not generally a particularly offensive smell. If you are having problems with excessive gas but it is not especially smelly, and you’ve been eating beans or peas, then they are almost certainly the culprit. On the other hand, if offensive flatulence odor is the problem rather than the volume of gas, it’s more likely to be one of high sulfur meat, eggs or veggies such as alliums (onion and garlic) or the cruciferous vegetable above or processed foods and drinks with sulfite preservatives - look for number 220-228 in ingredients - such as dried fruit and vegetables, condiments, and wine, cider and beer. Before you give up on cruciferous vegetables, it may be interesting to know that their pungent aroma and bitter flavor comes from sulfur-containing chemical in these vegetables known as glucosinolates. While human studies are inconclusive, glucosinolates have impressive cancer preventing properties in lab experiments.
Sugar alcohols (“polyols”) are also hard to digest and when take with fructose it is even harder. They are a common cause of intestinal gas and diarrhoea. The most common polyol is sorbitol. On the positive side, polyols contain less calories (1.5 – 3 calories per gram) than sugar (4 calories per gram), and they cause less tooth decay than sugar. Therefore, many “sugar-free” gums including Trident® and Extra®, lollies, mints and toothpaste are made with polyols instead of simple sugar. Fructose and sorbitol may be found together in some medications. Unfortunately, bowel side effect are common when taken in excess including bloating, flatulence, diarrhea, a “laxative effect,” and weight gain. Some people with diabetes have found that their blood sugars rise. Read labels as sorbitol is commonly hidden in many processed foods. Like all FODMAPs, raffinose, galacto-oligosaccharides and polyols are okay in moderation but should not be eaten in excess.
Group B: Lactose and Lactose intolerance 
trial a low lactose diet and use 3 Lacteeze enzymes with every dairy serve for 2 weeks minimum
decrease: cow’s milk (regular and low fat), ice cream, soft cheese (ricotta, cottage, cream cheese), yoghurt (regular and low fat), custard, evaporated/condensed milk
Try alternatives on diet A: lactose free cow’s milk (Liddel’s, Zymil), almond, oat, coconut or rice milk, goats milk; mature hard cheeses (Cheddar, parmesan); Gelato or sorbet (up to 1/3 cup standard milk may be tolerated in many), soy milk (not the whole soy varieties, i.e. soy protein only)
Dairy is important for calcium, protein and strong bones. However, for some, drinking milk or eating ice cream, a pizza or rich cheese causes bowel symptoms. This is usually a reaction to lactose - the natural sugars in dairy products. From about aged 7 most of the world’s population has lactose intolerance, so it is not a disease. It is common in people from Southern European, Asian, Middle Eastern and African backgrounds, and less common in northern Europeans. It may be temporary after viral infections, toxins, Giardia and gastroenteritis. Common symptoms include abdominal pain, bloating, flatulence and watery diarrhea.
Those with lactose intolerance have a deficiency of the digestive enzyme called lactase. Two sugar molecules, glucose and galactose, are bound together to form lactose. Before this sugar can be digested it needs to be broken in two by the enzyme lactase found in the wall of the small intestine. Without these lactase enzymes, lactose passes through the bowel undigested. Once in the large bowel, it provides nutrients for the gut flora, producing gas and other symptoms.
A low lactose diet is not a dairy free diet. It is important to learn which cheese, milk and yoghurt has less lactose. When dairy or lactose avoidance is not possible or not wanted, take 3 lactase enzyme supplements (tablets or liquid eg. 3 “Lacteeze” tablets). This often how manifacturers make lactose free dairy by dropping lactase into their lactose-full dairy products. "Lacteeze " tablets require a bit of practice to be effective but with trial and error many find them helpful. Eating yoghurt 15 minutes before milk may have the same effect for some.
"Slowly creeping up”: for many people, lactose intolerance fluctuates or may be temporary. By eating small amounts of dairy daily, the body may adjust by producing enough lactase enzymes with time to allow good tolerance without distressing symptoms. If dairy is not for you, be careful to get enough calcium and vitamin D for strong bones. You might ask your doctor to check your vitamin D level and if you need to take a calcium or vitamin D supplement.
Cheese and Butter: Traditionally hard and matured/aged cheese (like parmesan or mature cheddar), 'ripened' cheeses (such as brie, camembert and feta), Swiss or cottage cheeses and butter are low in or free from lactose. Cream cheese, ricotta and haloumi cheese can be a problem with moderate amounts of lactose.
Milk: Lactose-free cow milk (eg. Brands “Zymil” or “Liddell’s”), goat, buttermilk or plant milks (rice, almond, hazelnut, oat) may be good substitutes. Try making your own almond or other nut milk. Many enjoy soy protein milk. However, whole soy contains FODMAPs and can cause similar symptoms in others. There are some soy protein only milks that some can tolerate. Some with milk intolerance may be intolerant of the fat or protein not lactose sugar in milk. For these trying A2 milk or low fat brands may help.
Yoghurt: Low-fat plain Greek style (or pot set brands) may be preferred to more fatty yoghurts (which stay in the acidic stomach longer killing the helpful lactase enzymes). Frozen yoghurt can be harder to digest. Take care with food products that say “milk solids added" as these may be high in lactose.
If you find you are better lactose free, try this Monash or "I hate you milk" website. Look at low lactose ways to get your calcium: tinned fish with edible bones, plant milks fortified with calcium, green leafy vegetables, some brands of tofu and some seeds and nuts like sesame or tahini, almonds and Brazil nuts and Parmesan or Cheddar cheese.
Group C: Fructans: Wheat and onion intolerance and other oligosaccharides
Try low wheat, garlic and onions 2 weeks minimum
decrease fructans: Wheat (bread, cereal, pasta, biscuits), rye, onion (brown, white, white of spring, spanish, shallots), leeks, artichokes, zucchini, raddicio lettuce, chicory, Ecco/Caro drinks, Dandelion Tea, Inulin (artificial fibre added to products, e.g. dairy foods), Fructooligo saccharides (FOS) (artificial fibre added to some nutritional supplements)
Try alternatives: garlic infused oils; gluten-free products (cereal and bread); spelt bread, quinoa, chilli, chives, pinch of asafetida (indian spice market for onion flavour), ginger, spices, green of spring onion, fresh herbs (parsley, coriander, thyme, basil, rosemary); oats, rice and rice-based products; or small amounts of diet C
Oligosaccharides are dietary sugars joined together in microscopic small chains. They are either fructose- (fructo-oligosaccharides FOS/fructans) or galactose- based (galactans ie. galacto-oligosaccharides GOS). If you have trouble with onion and garlic you may have trouble with the sugars galactans. You are in good company as all mammals absorb galactans and fructans poorly. In susceptible individuals, these may cause distressing bowel symptoms. Food with longer sugar chains may cause fewer bowel symptoms than food with shorter chains. For example, rye crackers (rye has longer fructans) may be gentler on the stomach than bread (wheat has shorter fructans). Fructans are sometimes added to foods such as yoghurt. If you are vegetarian then restricting galactans (such as beans and legumes) may require a dietitian’s advice to help protein substitution. Several individuals avoiding wheat with self-diagnosed gluten intolerance, on further testing, have fructan carbohydrate not gluten protein intolerance.
Diet D (with diet A): Fructose Intolerance
Trial Low Fructose diet 2 weeks minimum
decrease fructose: Honey, tree fruits, melons eg. dried fruits (raisins, figs, peaches, prunes, apricots), fruit juice or concentrate, fruit pastes and sauces (tomato paste, chutney, relish, plum sauce, sweet and sour sauce, barbecue sauce); fortified wine (sherry, port), grapes, persimmon, lychee, apples, pears, mandarin, peach, guava, mango, watermelon, honeydew melon, pawpaw/papaya, quince, Lychees, Carambola, star fruit/carambola, Nashi fruit, Coconut cream/ coconut milk; Tinned fruit in natural juice (pear juice), Fructose or corn syrup products (ketchup, fruit drinks, carbonated drinks, pancake syrups, jams, jelly, pickle, relish, liquid cough remedies, some liquid medicine).
Try alternatives: banana, lemon, lime, orange, or small amounts of diet D including melons, grapefruit, grapes, kiwifruit, strawberries, pineapple etc.
Fructose intolerance is common and everyone has their threshold. So it is the amount of fructose in one serving is important. If you have a sensitive stomach, less than 25 g (a cup of dried figs) might cause distress, whereas for those with an “iron stomach,” eating more than 50g (eg. a cup of raisins, or 2 mangoes) may produce no symptoms at all. Small amounts of fructose (up to 3g) in one sitting are often well tolerated. If fructose and glucose are present in equal amounts more may be tolerated eg. a whole orange (3g) or 100ml orange juice (8g) or a tablespoon of dried fruit may be well tolerated, yet a cup (300ml) of orange juice (24g) or 5 prunes (14g) may cause symptoms.
| Fruit | Serving SIZE | Grams of Fructose |
| Figs, dried | 1 cup | 23 |
| Apricots, dried | 1 cup | 16.4 |
| Mango | 1/2 medium | 16.2 |
| Grapes, seedless (green or red) | 1 cup | 12.4 |
| Raisins | 1/4 cup | 12.3 |
| Pear | 1 medium | 11.8 |
| Watermelon | 1/16 med. melon | 11.3 |
| Persimmon | 1 medium | 10.6 |
| Apple (composite) | 1 medium | 9.5 |
| Date (Medjool) | 1 medium | 7.7 |
| Blueberries | 1 cup | 7.4 |
| Banana | 1 medium | 7.1 |
| Honeydew | 1/8 of med. melon | 6.7 |
| Papaya | 1/2 medium | 6.3 |
| Orange (navel) | 1 medium | 6.1 |
| Peach | 1 medium | 5.9 |
| Nectarine | 1 medium | 5.4 |
| Tangerine/mandarin orange | 1 medium | 4.8 |
| Boysenberries | 1 cup | 4.6 |
| Grapefruit | 1/2 medium | 4.3 |
| Cherries, sweet | 10 | 3.8 |
| Strawberries | 1 cup | 3.8 |
| Star fruit | 1 medium | 3.6 |
| Blackberries | 1 cup | 3.5 |
| Clementine | 1 medium | 3.4 |
| Kiwifruit | 1 medium | 3.4 |
| Raspberries | 1 cup | 3 |
| Cantaloupe | 1/8 of med. melon | 2.8 |
| Date (Deglet Noor style) | 1 medium | 2.6 |
| Guava | 2 medium | 2.2 |
| Apricot | 1 medium | 1.3 |
| Prune | 1 medium | 1.2 |
| Passionfruit | 1 medium | 0.9 |
| Cranberries | 1 cup | 0.7 |
| Lemons | 1 medium | 0.6 |
| Limes | 1 medium | 0 |