Preparing for colonoscopy
What is a colonoscopy?
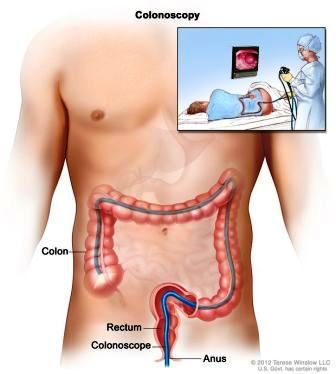
A colonoscopy is a short day procedure used to examine the lining of the lower part of the digestive tract.
Under sedation, the doctor passes a thin, flexible tube with a camera into the rectum and gently guides it along the colon to where it meets the small intestine. The doctor uses air to gently inflate and deflate the bowel to allow clear views.
A magnified image of the inside of the colon appears on a screen during the test.
The procedure itself usually takes about 20 minutes. You should plan to spend 2 to 4 hours at the clinic to allow time for waiting, preparation, and recovery. Bringing a book or something to read can help pass the time.
Who is responsible?
Dr Douglas Samuel will perform your colonoscopy. He has performed well over 10,000 colonoscopies.
An experienced team led by an anaesthetist will manage your sedation and look after your comfort and safety throughout the procedure.
Most people receive light “twilight” sedation rather than a full general anaesthetic. This usually means you sleep through the procedure and have little or no memory of it.
The anaesthetist adjusts the level of sedation carefully to keep you comfortable and safe. They can make it lighter or deeper if needed. You may briefly wake at times, but we will ask about your preferences and keep you comfortable throughout.
Preparation: What to Do Before Your Procedure
When you book your colonoscopy, you will receive an endoscopy session time (for example, Monday afternoon, 5 September, 1–6 pm). Occasionally, we may need to contact you to change this time.
If you need to change or cancel your booking, please call my rooms as soon as possible. This helps us offer your time to someone else on the waiting list.
Our staff will schedule your procedure at one of the following endoscopy units:
1. North Shore Private Hospital (NSPH)
Please complete the online admission form at least 3 working days before your test.
If you prefer paper admission forms (available from our rooms), please deliver them to the NSPH reception or the NSPH bookings department. You can return them by:
Fax: (02) 8425 4121
Email: nspbook@ramsayhealth.com.au
Mail or in person
For any hospital billing enquiries, please contact the NSPH billing department on (02) 8425 3000.
NSPH staff will call you to confirm your admission time on the afternoon before your test (between 3–6 pm), or on Friday if your procedure is scheduled for a Monday.
Dr Samuel or our practice nurse, Sr Jenny Burns RN, will contact you a few days before and after your procedure to help you prepare and to provide extra support.
The NSPH Day Surgery Unit is located in the Health Hub building. Entry is via Reserve Road or Westbourne Street. Take the Tower A lifts to the podium level and follow the signs to the Day Surgery Unit. Click below for the online admission form and a Patient Journey Video:
2. North Shore Specialist Day Hospital (NSSDH)
Please complete the online admission form (preferred method).
If you would prefer to complete a paper admission form (downloadable or available from our rooms), please return it at least 7 days before your procedure to the NSSDH admissions coordinator, Kim or Young Hee.
You can contact NSSDH by:
-
Phone: (02) 9425 1678
-
Fax: (02) 8088 6777
-
Email: admin@nssdh.com.au
NSSDH staff will call you to confirm your admission time on the afternoon before your test (between 2–5 pm), or on Friday if your procedure is scheduled for a Monday.
Our practice nurse, Sr Jenny Burns RN, will call you a few days before your procedure to help you prepare for the day.
3. Mayo Private Hospital (MPH) and Forster Private Hospital (FPH)
Please complete the online Pre-Admission Form. This usually takes about 30 minutes to complete.
If you have any problems completing the form, or if you would prefer to fill out a paper version, please contact:
Mayo Private Hospital (MPH)
-
Phone: (02) 6539 3600 (option 1)
Forster Private Hospital (FPH)
-
Phone: (02) 6555 1555
The hospital preadmission nurse, Sr Donna Chant RN is available a few days before your procedure to help you prepare for the day. If you have questions, please call the hospital and speak to Dr Samuel's rooms or Sr Chant.
You will be contacted with your admission time on the day before your test (or on Friday if your procedure is scheduled for a Monday):
-
FPH: by 11:00 am
-
MPH: by 4:00 pm
Can I take my current medications?
Most medications (including aspirin) can be continued. Please bring an up-to-date list of all your medicines with you to hospital.
Make sure you tell our staff if you have:
-
Severe drug reactions or allergies, or a family history of anaesthetic problems
-
A need for antibiotics for dental procedures
-
Taken any of the following in the past 3 months: the oral contraceptive pill, prednisone, or inhalers (“puffers”)
Common medications
Oral contraceptive pill
Use another form of contraception for 2 weeks after your procedure.
Iron or Anti-diarrhoea tablets
Stop 7 days before your procedure.
Asthma or steroid preventers / puffers
Use them at your usual or increased dose for 5 days before the procedure to ensure your lungs are at their best.
Blood thinners, diabetes medications, and weight-loss injections
If you take blood thinners, diabetes medications, or weight-loss injections, make sure your doctor has given you specific instructions. General guidance is below.
Antiplatelet medications
Aspirin
Take as usual. Do not stop.
Clopidogrel (Plavix®), prasugrel (Effient®), ticagrelor (Brilinta®)
Stop and switch to aspirin 100 mg for 7 days before the procedure.
Do not stop these medications without specialist advice if you have had a coronary angiogram with a stent or a heart attack within the past 6 months. In this situation, you may prefer to proceed without stopping them or postpone the colonoscopy until 6 months has passed.
Anticoagulants
NOACs (dabigatran [Pradaxa®], apixaban [Eliquis®], rivaroxaban [Xarelto®])
Stop 3 days before the procedure.
Warfarin or Clexane
Seek special instructions.
Do not stop anticoagulants without specialist advice if you started them within the past 3 months, especially if this was for a blood clot, DVT, or pulmonary embolism.
Diabetes tablets and insulin
For all diabetes medications (metformin, gliptins, gliclazide, SGLT2 inhibitors, insulin):
-
Do not take diabetes medications on the day of the test unless instructed
-
On the day before the test, take half your usual insulin dose
-
Be careful to avoid low blood sugar (“hypos”)
SGLT2 inhibitors (dapagliflozin [Forxiga®], empagliflozin [Jardiance®], ertugliflozin [Steglatro®] and combinations such as Xigduo®, Jardiamet®, Segluromet®, Glyxambi®, Qtern®, Steglujan®)
Stop 3 days before the procedure.
You will usually be placed first on the list on the day of your procedure.
Weekly weight-loss / diabetes (GLP-1) injections
Includes dulaglutide (Trulicity®), semaglutide (Ozempic®, Wegovy®), tirzepatide (Mounjaro®), liraglutide (Victoza®, Saxenda®), retatrutide
Stop 1 week before the procedure, if possible.
Because bowel preparation can be poorer with these medications:
For 5-7 nights before:
-
Take 2 senna or bisacodyl every night, or
-
If you already take something for constipation, double your usual dose (for example, Movicol or senna)
Risks and Safety
Before your procedure, you will have an opportunity to ask questions about the benefits and risks of your colonoscopy. Your doctor will answer these in a way you can understand.
Colonoscopy is a very safe procedure. Nausea and bloating are common after taking bowel cleansing laxatives, but these symptoms usually go away quickly.
If the bowel is not clean, or your anatomy makes the test difficult, the doctor may not be able to complete the procedure. In this situation, your doctor may recommend repeating the procedure on another day, arranging another test, or deciding that the limited examination is sufficient.
To maximise your chance of a good bowel preparation, follow the bowel cleansing instructions carefully. This includes taking the laxatives 4–5 hours before afternoon procedures and not following the timing printed in the Prepkit Orange packet.
Even with the best techniques, small polyps or tumours can occasionally remain hidden from view and may be missed.
Possible complications
Complications that require urgent surgery are rare (about 1 in 1,000).
In some people, the bowel wall is unusually fragile and can puncture or bleed. Bleeding after polyp removal is usually minor and often stops on its own.
Other uncommon problems include reactions to the sedative or bowel preparation, infections, or worsening of existing heart or lung disease.
You may feel a brief stinging or “sparkle” sensation in your arm from the intravenous sedative. Some people wake with a sore angle of the jaw if the anaesthetist needs to apply pressure there to keep breathing safe during the procedure. This jaw tenderness usually settles after a few days.
Aspiration-related chest infections, which means breathing fluid into the lungs during sedation, are uncommon, particularly if your stomach is empty and you have fasted as instructed.
When to seek medical help
Although complications are uncommon, it is important to recognise them early.
Contact your doctor or hospital if you notice:
-
Severe abdominal pain
-
Dizziness
-
Fever or chills
-
Rectal bleeding (more than half a cup)
-
Severe shortness of breath
Bleeding risk and travel after polyp removal
Your risk of major bleeding after polyp removal continues for up to 10–14 days, with the greatest risk in the first 48 hours.
We do not recommend air travel:
-
For domestic flights within 48 hours of polyp removal
-
For long-haul flights or travel to remote areas within 5 days if a polyp has been removed
Are there alternatives to colonoscopy?
Doctors consider colonoscopy the best test because it allows diagnosis and treatment at the same time and plays a key role in bowel cancer prevention and the detection of polyps.
Other tests, such as CT colonography or stool-based tests, may have a role in some situations. You can discuss these options with your doctor to help choose the most appropriate test for you.
What about COVID or recent illness?
If you’ve been unwell recently, we just need to make sure it’s safe for you to go ahead with your colonoscopy and sedation. You can usually continue with your bowel preparation and procedure without delay if:
- Your rapid antigen (RAT) test is negative
- It’s been more than 4 weeks since a mild COVID infection or mild heart or lung illness
- It’s been more than 8 weeks since you were in hospital for a chest infection, breathing, or heart problem
- You are COVID-negative twice – once during bowel prep and again on the day of your procedure
- You have only mild cold or flu symptoms, with a negative PCR (within 3 days) and a negative RAT on the day of your procedure
- You can comfortably climb two flights of stairs while carrying shopping without getting short of breath or chest pain
If you’re unsure, or if any of these don’t apply, please let our staff know. We’ll review your situation and make sure your procedure can go ahead safely.
Bowel cleansing: in 3 steps
Quick prep summary: This is usually the most troublesome part of your procedure
48–24 hours before your colonoscopy
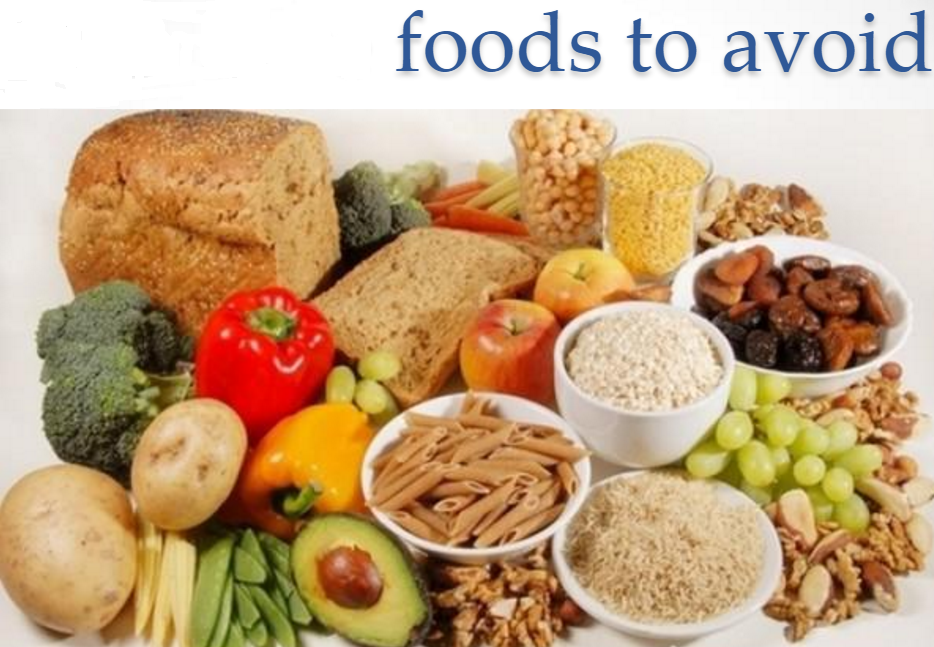
The “white diet” (low fibre / low roughage)
Golden rule: do not eat it if it has seeds (including bread with seeds), skins, nuts, wholegrains, uncooked vegetables, or fibre
You may eat
Grains and cereals: White rice, white bread, white pasta, Rice Bubbles, Cornflakes, congee.
Meat, fish, and eggs: Fresh white fish, poultry (no skin), bacon, pork or chicken sausage, eggs (use one yolk only, for example scrambled whites with one yolk).
Vegetables: Boiled peeled potatoes or pumpkin, potato salad (no skin or greens), hash browns, canned or well-cooked vegetables without skins or seeds.
Dairy (if tolerated): Milk, plain yoghurt, butter, margarine, ice cream, chocolate, cream, cottage cheese, ricotta, or feta.
Meals, breads, and breakfasts: Macaroni cheese, pasta carbonara (no tomato or bottled sauces), plain white pasta with butter or cheese, plain white rice with butter, plain bagels or white toast with Vegemite, honey, lemon butter or butter, French or cinnamon toast, plain or ham/cheese croissants, plain cheese toasties (white bread only), crumpets, pancakes, waffles or pikelets with lemon, sugar, or honey, scones with honey, chocolate brioche, plain muffins (no fruit, seeds, or nuts).
Snacks and extras: Rice custard, chocolate mousse, cheese with crackers or rice cakes, protein bars (no nuts or seeds), wedges with sour cream, ham quiche, parmesan cheese sticks.
You may drink: All clear fluids listed in the next section.
If you usually eat raw fruit or vegetables, you may use a juicing machine to remove the pulp before drinking.
Do not eat (even if they look “white”): Pears, parsnip, cauliflower, onion, high-fibre white breads (for example Wonder White), tofu, coconut, porridge, banana, mushrooms, semolina, couscous, popcorn.
24–2 hours before your colonoscopy
Clear fluids only (no solid food)
Golden rule: If you can read a newspaper through it, it’s allowed.
You may drink:
-
Water, Clear fruit juices (apple, pear, white grape), coconut water,
-
Clear cordials (lemon or lime), Sports drinks (for example Gatorade®), Carbonated drinks
-
Black tea or coffee (or skim milk)
-
"Protein Water", Clear broth or bouillon, or Vietnamese pho broth (strain noodle soups; chicken, beef, or vegetable), Bonox
-
Honey, Popsicles, Sorbet or gelati, Jelly
- NOT within 4 HOURS BEFORE TEST: Ensure® Clear, Hard or gelatine sweets (for example barley sugars, lollipops, gummy bears)
-
NOT ON TEST DAY: Very thin congee, Small amounts of clear alcohol (light beer, white wine, vodka, gin, or whiskey) -
Do not have:
-
Any solid food
-
Full-cream milk
-
Any red, or purple food colouring (for 24 hours before the test) in your fluids
Take care to avoid dehydration.
Aim to drink 2–3 glasses or serves of clear fluids at:
-
Breakfast
-
Morning tea
-
Lunch
-
Afternoon tea
-
Dinner
-
Evening
-
And on the morning of the test, up to 2 hours before your appointment

Bowel cleansing (Prepkit Orange)
Buy Prepkit Orange (3 sachets) well in advance from a local pharmacy.
No prescription is required. Your kit contains:
-
Picoprep (2 Green sachets, picosulfate)
-
Glycoprep (1 Orange sachet, macrogol)
How to mix and drink each sachet
Picoprep
Add one sachet to one 250 mL glass of warm water. You can chill it in the fridge before drinking if you prefer. Drink it over 30 minutes.
Glycoprep
Add the sachet to four 250 mL glasses (or a 1 litre jug) of warm water. You can chill it in the fridge before drinking if you prefer. Drink one glass every 15 minutes. If you start to feel nauseous, slow down.
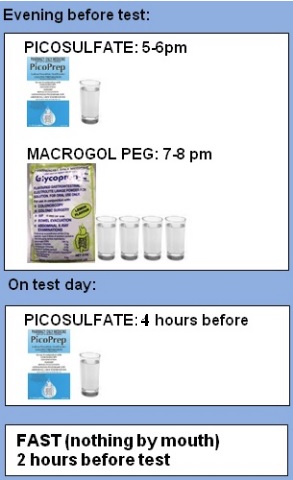
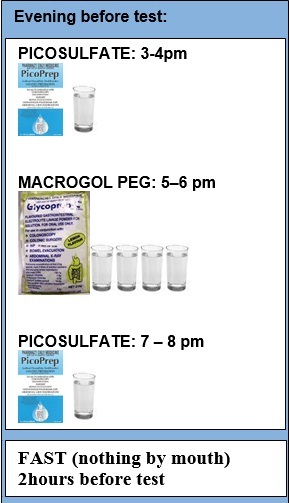
How many sachets to take and when
You will take two sachets the evening before your procedure and one sachet on the day of the test.
After each sachet, expect diarrhoea to start anywhere from 30 minutes to 4 hours later.
Timing depends on your appointment time
If your colonoscopy is after 10:00 am
Use a split-prep schedule:
-
Take two sachets the evening before
-
Take one sachet on the morning of the test, finishing at least 4 hours before your appointment
(This gives the best bowel cleansing and is strongly recommended.)
If your colonoscopy is before 10:00 am
Your options for the third sachet (Picoprep number 2) depend on when you prefer to sleep. You can take it:
-
At 3:00 pm the day before
(for example: sachets at 3 pm, 5 pm, and 7 pm) — this is the most common option -
At 9:00 pm the day before
(for example: sachets at 5 pm, 7 pm, and 9 pm) -
Four hours before your procedure
(for example: for an 8:00 am test, take sachets at 5 pm and 7 pm the evening before, then set an alarm and take the final sachet at 4:00 am). This requires commitment, but gives the best possible bowel cleansing.
Buy Prepkit Orange (3 sachets) well in advance from a local pharmacy
(No prescription required):
"PICOPREP" (x2 picosulfate): add (sachet A or C) to ONE 250mL glass of warm water (if preferred, chill in a refrigerator before drinking), drink over 30 minutes
"GLYCOPREP" (x1 macrogol): add (sachet B) to FOUR 250mL glasses (or 1L jug) of warm water (if preferred, chill in a refrigerator before drinking). Drink 1 glass every 15 mins. If you start to feel nauseous, slow down
take two sachets the evening before and one on test day
Expect diarrhoea (30 mins to 4 hours) after drinking laxative sachet
FOR COLONOSCOPY AFTER 10AM*
FOR COLONOSCOPY BEFORE 10AM*
* FOR COLONOSCOPY BEFORE 10AM
Your options for the third sachet (Picoprep no. 2) depend on when you like to sleep. They are to take it:
- at 3pm (ie take each at 3pm, 5pm, 7pm)- most common
- at 9pm (ie take each at 5pm, 7pm, 9pm)
- 4 hours before (ie. for a 8am test, with serious committment to best-in-class split prep, after setting your alarm,take sachets at 5pm, 7pm and the next day at 4am! )
Ten tips for surviving bowel prep and “colon photo shoot”
-
Prepare your laxative mixtures in advance and chill them well.
-
If you feel nauseous, slowing down is usually enough. If severe nausea or vomiting is a concern, ask your doctor for ondansetron (Zofran) to take one hour before the first laxative dose and then every six to eight hours during the process. This is effective for most people.
-
You can add lemon juice, ginger ale, or lime cordial to improve the taste (but only if you never want to drink that beverage again in your life).
-
Chill the glass, drink with a straw, and rinse your mouth after drinking.
-
Suck on sweets between drinks.
-
Stock up beforehand on peppermint tea, lemonade ice blocks, and ginger ale.
-
Apply Vaseline or zinc oxide to the anal area in advance, and use baby wipes instead of toilet paper.
-
Make sure your bathroom is safe and well lit, especially at night, to prevent falls or accidents.
-
Do not be afraid to bring some entertainment to the bathroom — you will be there for a while.
-
Drink clear fluids right up to 2 hours before your test (unless you have been told otherwise).
If you feel you would be more comfortable being admitted the night before your colonoscopy for extra nursing care, please let our rooms know.
For our Sydney patients, Sr Jenny Burns RN, our North Shore endoscopy practice nurse, will give you her number when she calls before and after your procedure. She is available if you would like to talk about your procedure or bowel preparation. You can also contact the hospital to speak with the endoscopy nurses.
Special instructions for some groups
Some people need a little extra attention and specific instructions for bowel preparation.
You may need special instructions if you have any of the following:
Colonoscopy before 10:00 am
If your colonoscopy is scheduled before 10:00 am, follow the timing instructions outlined above for early procedures.
“Bowel prep PLUS” (extra preparation)
You may need an enhanced bowel preparation (including taking increased daily laxatives for 7 days before the procedure) if you have:
-
Diabetes
-
Severe constipation
-
A previous colonoscopy with inadequate bowel preparation
Moviprep or Plenvu only - PEG/macrogol-based (Picoprep free)
These preparations are preferred if you have:
-
Severe kidney disease (eGFR < 30)
-
Liver cirrhosis (especially if taking spironolactone)
-
Heart failure (if taking frusemide or spironolactone, or if ejection fraction is below 40%)
"Bowel Prep in a capsule" or Prep thickener - if liquid preparation is difficult
If you have trouble tolerating liquid bowel preparations, options may be considered if you have:
-
Difficulty swallowing or require grade 1–2 thickened fluids
-
Intolerance of liquid prep, where capsule-based options or anti-nausea medication may help
If any of these apply to you, please let our rooms know so we can give you the most appropriate and safe preparation plan.
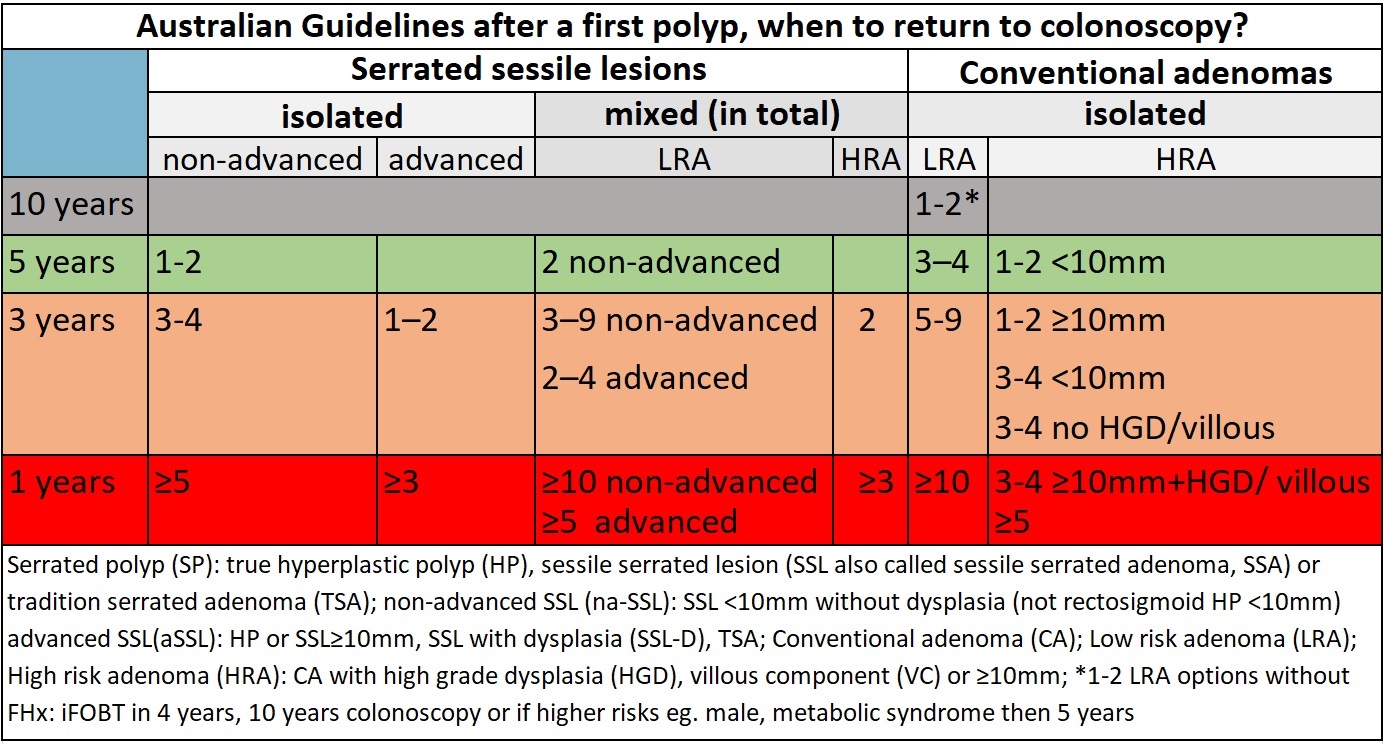
What if something abnormal is found?
If an area needs further testing, a biopsy will be taken. This is a very small sample of the colon lining, about the size of a grain of rice.
If there is any bleeding, it can usually be controlled during the procedure using special techniques.
If polyps are found (benign growths on the lining of the colon), they are usually removed at the same time. This is called a polypectomy. Removing polyps is an important way to help prevent bowel cancer.
Biopsies and polyp removal are not painful.
If haemorrhoid bleeding or discomfort is a significant problem, you can ask about treating this during the procedure while you are sedated. Non-surgical options include rubber band ligation or infrared coagulation.
These haemorrhoid treatments usually involve less pain and lower risk than surgery, but they can cause short-term pain or discomfort for a few hours to a few days. You will need to give consent before your sedation if your doctor is going to treat haemorrhoids.
After the colonoscopy: recovery and results
When you wake up, you may feel wind pain, bloating, and pass air that was introduced during the test. You may also have some discomfort at the vein access site on your arm.
Even if you feel alert, your judgement, memory, and reflexes will be impaired for the rest of the day.
Your doctor will see you after the test and discuss the results with you, and you will be given a written report. It is common to have little or no memory of the test or this discussion.
Someone you know must drive you home and stay with you after the procedure. Hospital policy does not allow taxi services.
Until the next day, do not:
-
Drive a car
-
Sign legal papers
-
Send important emails
-
Drink alcohol
-
Operate machinery
A report including any biopsy results will be sent to your referring doctor after about one week.
It is important that you contact our rooms to make, and keep, a follow-up appointment with your specialist or referring doctor to discuss your results.