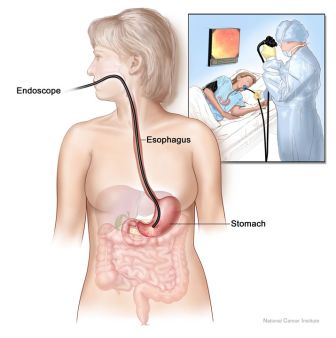
What is a gastroscopy?
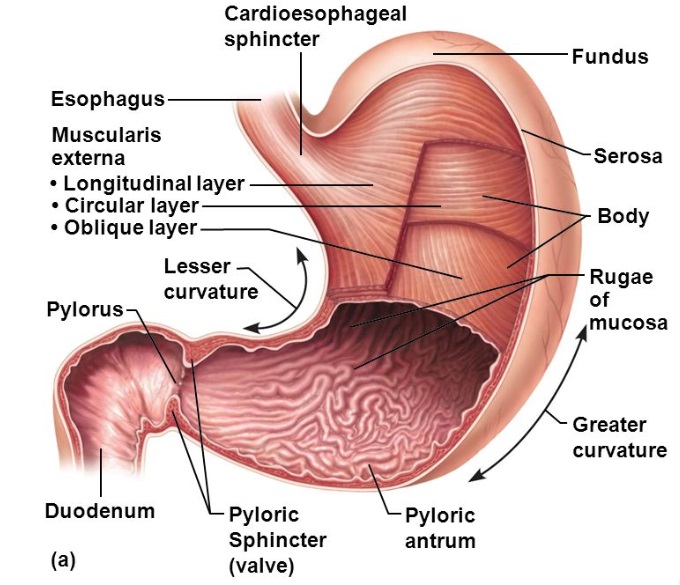
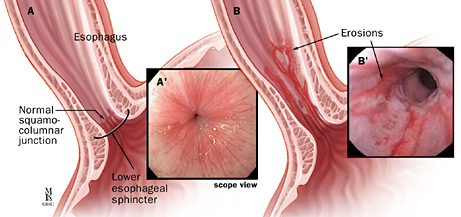
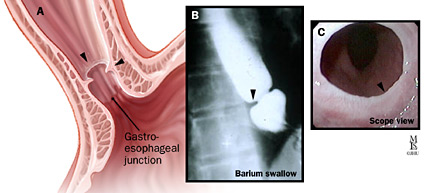
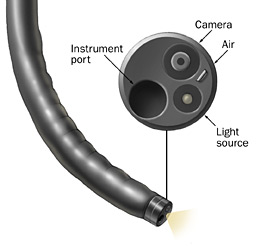
This is a short procedure to examine the lining of the upper part of the digestive tract. Under sedation, a thin flexible tube camera is place into the mouth and gently moved along the food path along the oesophagus (gullet), stomach and beyond to the duodenum. A magnified image of the upper digestive tract’s inner surface is projected on a TV screen. It helps find reasons for swallowing, digestion difficulties, nausea, vomiting, heartburn, abdominal fullness, indigestion, bloating, abdominal or chest pain. Ulcer bleeding, Barrett’s oesophagus, varices, narrowings or polyps may be treated at the time. The test takes about 10 minutes. Plan 2 - 3 hours for waiting, preparation and recovery and bring a good book.
Who is responsible?
Dr Douglas Samuel will perform the test. An experienced team lead by an anaesthetist will sedate you and ensure your comfort and safety.

1. North Shore Private Hospital (NSPH) Day Surgery Unit
Please complete online admission form at least 3 working days prior to your test. If you prefer paper admission forms (available from our rooms), please deliver papers to NSPH reception or the NSPH bookings department (fax: 8425-4121; mail or email: nspbook@ramsayhealth.com.au). NSPH staff will call to confirm your admission time on the afternoon 3-6pm before your test (or Friday for a Monday test). Please contact NSPH billing department for any hospital billing inquires (tel: 84253000). Dr Samuel or our practice nurse Sr Jenny Burns RN will contact you a few days before and after your procedure to help you prepare for the day and provide you with extra support. The NSPH Day Surgery unit is located in the Health Hub building, entry is via Reserve Road or Westbourne Street, take the Tower A lifts to the podium level and follow the signs to Day Surgery.
2. North Shore Specialist Day Hospital (NSSDH): Please download and forward completed online admission form to NSSDH admissions coordinators, Kety Lucic or Kim Butler (tel: 9425 1678; fax: 80886777; email: info@nssdh.com.au) at least 5 working day prior to your test. If you have not already delivered your admissions form, please submit these to Kety or Kim on the day of your admission. NSSDH will call to confirm your admission time on the afternoon (2-5pm) before your test (or Friday for a Monday test). Our practice nurse sister Jenny Burns RN will call you a few days before your procedure to help prepare you for the day.
3. Mayo (MPH) and Forster Private Hospital (FPH)
Please complete the online Pre-Admission Form here. This form should take you approximately 30 minutes to complete. If you have any problems completing the form or would like fill out the paper version, please contact: the MPH admissions coordinator via: mayo.admissionforms@healthecare.com.au or 65393600 option 1; or for Forster Private Hospital the FPH day surgery coordinator via: ftr.admissions@healthecare.com.au or 65551555. Our practice nurses sister Donna Chant RN (MPH) or Katrina Hansen RN (FPH) will call or see you a few days before your procedure to help prepare you for the day. You will be contacted with your admission time the day (FPH by 11am, MPH by 4pm) before your test (or Friday for a Monday test).
What preparation is required - "the 6-4-2 rule"?
For sedation and adequate views, your stomach must be empty. For gastroscopy, we follow the 6-4-2 rule. It is important you take no solid food by mouth from 6 hours and no fluids from 4 hours before. You may sip WATER ONLY up to 2 hours before. The only exception is that you make take all your usual medicine with a sip of water. If you are on a "GLP1-RA" injectable medication for diabetes or weight loss [dulaglutide (Trulicity), semaglutide (Ozempic, Wegovy), terzipitide (Mounjaro) , liraglutide (Victoza, Saxenda)], it may take longer than 6 hours to digest the solid food in your stomach, so you need to begin the clear liquid diet 24 hours prior to your procedure.
Can I take my current medications?
Most medications (including aspirin) can be continued. Be sure to tell our staff i) your drug reactions or allergies, ii) if you need antibiotics for dental procedures and iii) if, in the past 3 months, you have taken: aspirin, blood thinners (eg. warfarin, clopidogrel, rivaroxaban), insulin or prednisone. If you are on the “pill,” use another contraceptive for 2 weeks after your procedure. Stop anti-diarrhoea or iron pills five days before. If you use steroid puffers for asthma, use them at usual or increased dose for 5 days before the procedure. If you take diabetes pills or insulin - then on test day, these must not be taken unless instructed - on the day before the test, take half the usual insulin and be careful with “hypos”. Bring an up-to-date list of all your medicines to hospital.
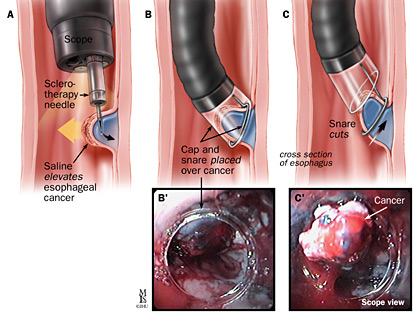
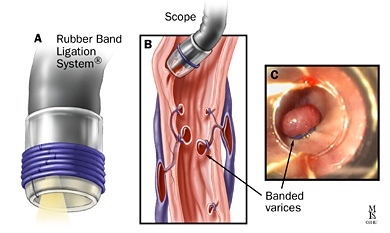
What if something abnormal is found?
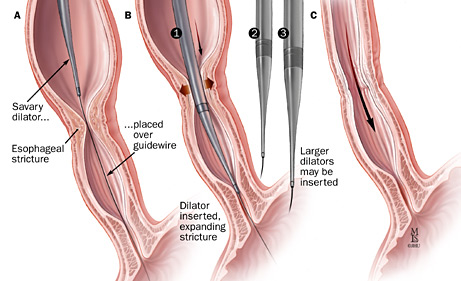
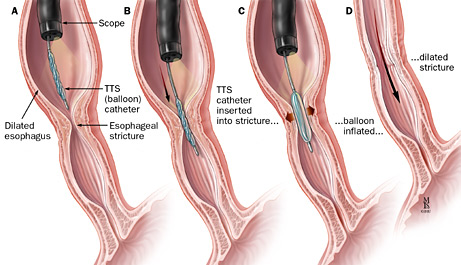
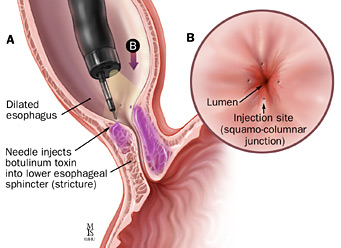
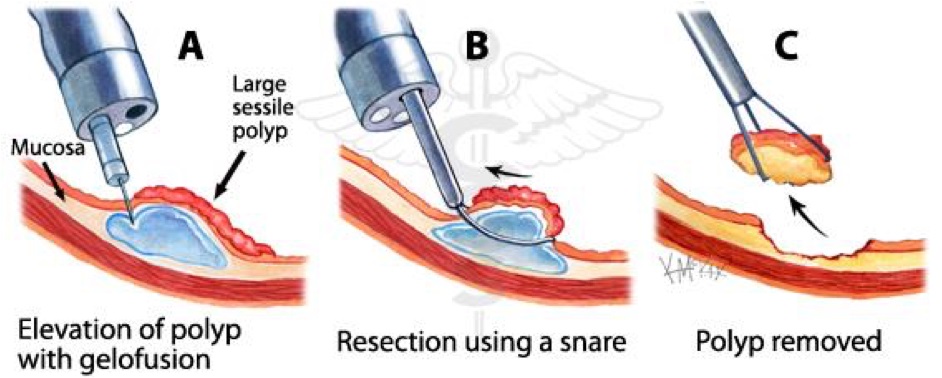
If an area needs further testing, you will have a biopsy (a rice grain-sized sample of tract lining). Unexpected bleeding problems may be controlled with special coagulation or clipping techniques. With other uncommon finding, other special non-urgent procedures may be performed only with your prior consent. These findings include: strictures (narrowings or blockages) which may be dilated with a balloon or dilator; large polyps (benign growths on the stomach lining) which may be removed by snare polypectomy; oesophageal varices (varicose veins in the gullet) which may be treated with rubber band ligation. Biopsy and these special procedures are usually painless.
What are the risks?
Before your procedure, you will have an opportunity to ask questions particularly about the benefits and risks of your gastroscopy and have these answered in a way that you understand. Gastroscopy is very safe. Complications needing urgent surgery are rare (1 in 15000). Dr Samuel may treat several conditions including swallowing difficulties with dilatation or stenting of narrow segments (strictures), thermocoagulation of bleeding vessels or ulcers, banding of dilated variceal vessels, removal of polyps or foreign bodies, Botox injection to segmental spasm. Each of these have special risks which Dr Samuel will discuss with you. Other uncommon problems include sedative reactions, infections or worsening of existing heart or lung disease. Although complications are uncommon, it is important to recognise them early. Contact your doctor or hospital if you notice severe abdominal pain, dizziness, fever, chills, black motions, severe shortness of breath or vomit blood.
Are there alternatives?
Gastroscopy is considered the best test for same time diagnosis and biopsy of internal tissue. Ultrasound and Xray techniques including CT scan or MRI and blood testing may have a role. Discuss the alternatives with your doctor to help choose.
What happens after gastroscopy?
On waking, you may feel wind pain, bloating and belch air introduced during the test. You may have discomfort at the vein access site on your arm. Even if you feel alert, your judgement, memory and reflexes will be impaired for the rest of the day. Your doctor will see you after the test and give you your results with a written report. It is common to have no memory of the test or discussion. Someone familiar must drive you home and stay with you after the procedure. Our hospital policy does not allow taxi services. Do not drive your car, sign legal papers or send important emails, drink alcohol or operate machinery until the next day. A report with biopsy results will be sent to your referring doctor after about a week. It is important that you make and keep a follow up appointment with your specialist to discuss the result.