
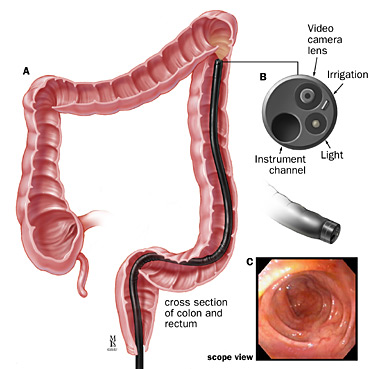
What is a sigmoidoscopy?
This is a short procedure to examine the lining of the lower sections of the colon - the lower part of the digestive tract. A thin flexible tube camera is passed into the rectum and gently moved along the first part (1-2 feet) of the colon (inflating then deflating with carbon dioxide or air). A magnified image of the left colon’s inner surface is projected on a TV screen. The test takes about 10 -15 minutes and is usually uncomfortable but not painful. Several patients who choose no sedation, say they would do it without sedation again if required. Sedation is available and is your choice. If sedated, plan 2 - 4 hours for waiting, preparation and recovery and bring a good book. With unsedated sigmoidoscopy, it is somewhat faster and you may drive immediately afterwards.
Who is responsible?
Dr Douglas Samuel will perform the test. Many choose the services of our anaesthetist who will be able to sedate you safely for extra comfort. However, a sigmoidoscopy is usually uncomfortable but not painful so you may choose not to have sedation as well. An experienced team ensure your comfort and safety either way.
What happens before the test?
On booking, you will be given an endoscopy session (eg. Monday afternoon 5 September 1-6pm). Occasionally, we may call you to change it. Dr Samuel or his nurse Sr Jenny Burns will contact you a few days before and after your test to support you as you prepare for the day. To change or cancel your booking, please call my rooms as soon as possible, to allow for others on the waiting list.
1. North Shore Private Hospital (NSPH): Please complete online admission form at least 3 working days prior to your test. If you prefer paper admission forms (available from our rooms), please deliver papers to NSPH reception or NSPH endoscopy bookings coordinator (tel: 84253875; fax: 84255622; email: Endobook.NSP@ramsayhealth.com.au). One of the booking coordinators will call to confirm your admission time on the afternoon before your test (or Friday for a Monday test). Please contact him for any hospital billing inquires. Our practice nurse Sr Jenny Burns RN will call you a few days before your procedure to help prepare you for the day.
2. North Shore Specialist Day Hospital (NSSDH): Please download and forward completed online admission form to NSSDH admissions coordinators, Kim Butler or her colleague (tel: 9425 1678; fax: 80886777; email: info@nssdh.com.au) at least 5 working day prior to your test. If you have not already delivered your admissions form, please submit these to Kim on the day of your admission. NSSDH will call to confirm your admission time on the afternoon (2-5pm) before your test (or Friday for a Monday test). Our practice nurse sister Jenny Burns RN will call you a few days before your procedure to help prepare you for the day.
3. Mayo Private Hospital (MPH): if you have not already delivered your admissions papers to MPH admissions coordinator, Jess McGuire (tel: 65520061 or 65393600 -option 5; fax: 65520059, email: jessica.northam@healthecare.com), please submit your admission papers on the day of your admission. You will need to call Jess to confirm your admission time on the afternoon (2-4pm) before your test (or Friday for a Monday test). Our practice nurse sister Donna Chant RN will call or see you a few days before your procedure to help prepare you for the day.
Can I take my current medications?
Most medications (including aspirin) can be continued. Be sure to tell our staff i) your drug reactions or allergies, ii) if you need antibiotics for dental procedures and iii) if, in the past 3 months, you have taken: aspirin, blood thinners (eg. warfarin, clopidogrel, rivaroxaban), insulin or prednisone. Stop anti-diarrhoea or iron pills five days before. If you use steroid puffers for asthma, use them at usual or increased dose for 5 days before the procedure. If you take diabetes pills or insulin - then on test day, these must not be taken unless instructed - on the day before the test, take half the usual insulin and be careful with “hypos”. Bring an up-to-date list of all your medicines to hospital.
What if something abnormal is found?
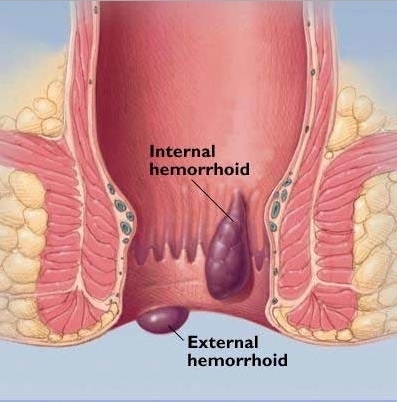
If an area needs further testing, you will have a biopsy (a rice grain-sized sample of colon lining). Bleeding problems may be controlled with special techniques. Usually, if you have polyps (benign growths on the colon lining) these will be removed called polypectomy. Polypectomy is an important way to prevent bowel cancer. Biopsy and polyp removal is not painful. If haemorrhoid bleeding or discomfort are a significant problem, ask about treating these while sedated with non-surgical techniques including rubber band ligation or infrared coagulation. These haemorrhoid treatments, while associated with less pain and risks than haemorrhoid surgery, may cause manageable short term pain or discomfort for a few hours to days.
What are the risks?
Before your procedure, you will have an opportunity to ask questions particularly about the benefits and risks of your flexible sigmoidoscopy and have these answered in a way that you understand. Sigmoidoscopy is very safe. Following the enema, bloating discomfort and cramps rarely lasts long. You may also feel an urge to go to the toilet or pass wind.can cause slight abdominal cramps in some people. Even with the best techniques, polyps and tumours can be hidden from view and missed. The bowel wall may be unusually fragile and puncture or bleed. Bleeding after polyp removal is usually minor and stops on its own. Complications needing urgent surgery are rare : 1 in 15000 for a diagnostic test only or 1 in 500 if polyps are removed. Other uncommon problems include sedative reactions, infections or worsening of existing heart or lung disease. Although complications are very uncommon, it is important to recognise them early. Contact your doctor or hospital if you notice severe abdominal pain, dizziness, fever, chills, rectal bleeding (more than 1/2 a cup) or severe shortness of breath. Bleeding can occur up to 14 days after a polyp removal.
Are there alternatives?
Sigmoidoscopy is considered a good test for same time diagnosis and treatment of polyps, inflammation and causes of bleeding from the bowel. It can be used as a bowel cancer scr

eening test to detect more common left sided cancers. Blood tests, CT scan and stool testing may have a role. Discuss the alternatives with your doctor to help choose.
What bowel cleansing is required?
This involves having an enema about 1/2 an hour prior to the test. This is usually the most troublesome part of your procedure. If you request sedation, you will need to fast before: 6 hours no solids, 4 hours no liquids, 2 hours no sips of water. If you are having it without sedation it is best if you don't eat or drink too much prior.
What happens after a flexible sigmoidoscopy?
On waking, you may feel wind pain, bloating and pass air introduced during the test. You may have discomfort at the vein access site on your arm. If you've had sedation, even if you feel alert, your judgement, memory and reflexes will be impaired for the rest of the day. Your doctor will see you after the test and give you your results with a written report. It is common to have no memory of the test or discussion. Someone familiar must drive you home and stay with you after the procedure. Our hospital policy does not allow taxi services. Do not drive your car, sign legal papers or send important emails, drink alcohol or operate machinery until the next day. A report with biopsy results will be sent to your referring doctor after about a week. It is important that you ring the rooms to make and keep a follow up appointment with your specialist to discuss the results.

