Special instructions for procedures: diabetes, blood thinners, preps
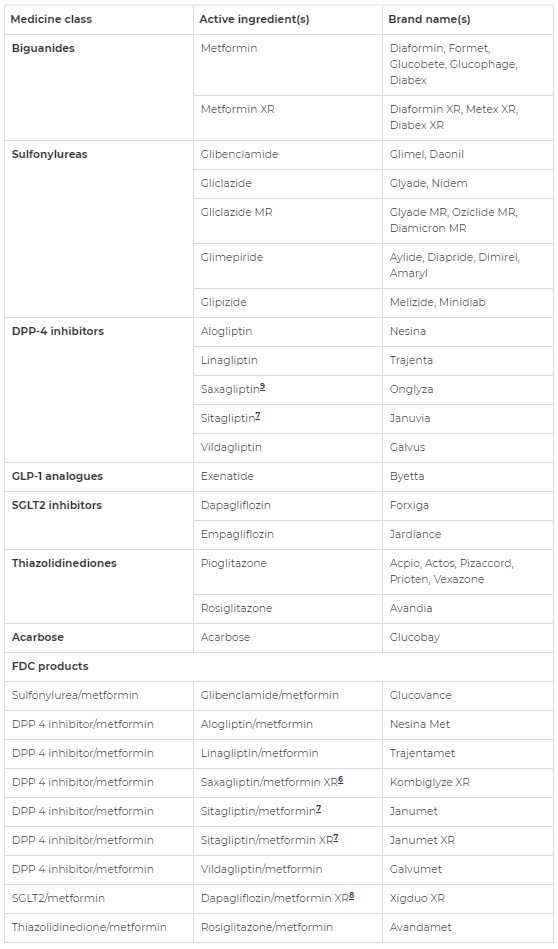
Diabetes
- Stop 3 days before your procedure
- SGLT2 inhibitors have been associated with an increased risk of diabetic ketoacidosis particular when fasting for procedures. It presents with normal or only mildly elevated glucose concentrations <14mmol due to loss of glucose in the urine.
- for referring doctors: " risk of ketoacidosis increased as SGLT2 inhibition results in a proketogenic state due to urinary caloric losses and a decreased insulin-to-glucagon ratio, stimulating lipid utilization; the superimposed effects of diet modifications, prolonged fasting when scheduled later in the colonoscopy list, bowel preparation, and not stopping SGLT2i precolonoscopy."
- It is therefore important that nurses test your urine for ketones on the morning of your test particularly if you feel unwell and regardless of your blood glucose concentration. Urine ketones >1-5 is normal in a fasting start. If ketones are >1 you will get a blood test to look for increased acid in your blood which is not normal.
- The Australian Diabetes Society has published recommendations based on expert opinion to try to reduce the risk of perioperative diabetic ketoacidosis. Recommendations include withholding SGLT2 inhibitors for 4 days before colonoscopy.
- These guidelines have been modified to 3 days with the understanding that colonoscopy is a short procedures with a shorter 2 hour fast. Stopping for 4 days might cause your sugars to increase. So you can choose 3 or 4 days.
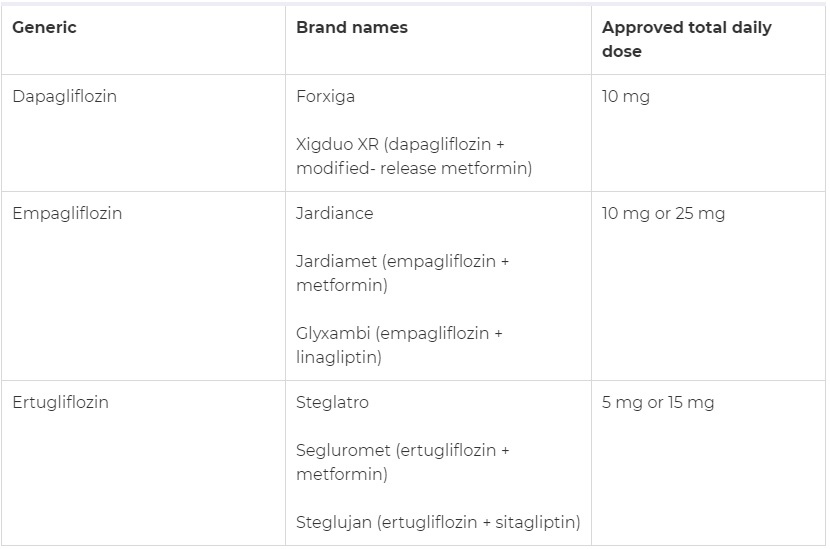
- You need to be very careful to keep up your hydration and keep up with fluids with carbohydrates when you take this type of diabetes medicine as there have been reports of acidosis during colonoscopy
- If you can guarantee good hydration including carbohydrates then stop 72 hours before: ie. take your 'flozin tablet as normal the evening of day -4. Stop all doses on day -3, day -2, the day before and on test day. eg. last dose Thursday for a Monday colonoscopy.
- If you are worried that you might not be able to keep up the recommended hydration on the day prior, then it is best you withhold this tablet for 4 days prior: three days prior as well as on test day. This may require talking to your doctor about increasing other glucose-lowering drugs during that time.
- On test day: take no diabetes tabs
- Restart these diabetes tablets in the evening after the test
- Reason: high risk of hypos on "free fluid"/no solid food on day before and day of endoscopy. Plus, with dehydration on these tablets you can develop symptoms of ketoacidosis include nausea, vomiting, abdominal pain, tiredness, and trouble breathing. If you get acidosis or these symptoms we will postpone your procedure or give you an insulin/dextrose infusion.
Special instruction:
- If BSL is >10 use broths or diet drinks, otherwise ensure fluids contain glucose particularly if BSL<5.
- If you have unstable diabetes or take high dose insulin then you may need to be admitted for an insulin-glucose infusion on the morning of the test
- More frequent BSL monitoring is essential and if you have unstable control you may need to monitor hourly
On the day prior to the colonoscopy:
- reduce short acting insulin to avoid "hypos":
take normal short-acting insulin at breakfast
at lunch take ½ (half normal short-acting insulin dose)
pre-bed take ½ (half usual long-acting insulin dose) - You should check your home glucose values every four hours
On the morning of the test:
- omit insulin until after procedure
- You should have been given the (first) early appointment on the list. (If you do not have an early morning appointment – please contact Dr Samuel's rooms or the hospital so that your appointment can be altered
- After the procedure take ½ (half) normal short-acting insulin with a snack and return to normal insulin doses from lunchtime or dinner onwards
- On the day prior to the colonoscopy take ½ (half) normal insulin doses at breakfast
- You should check your home glucose values every four hours
- On the day of the procedure omit morning insulin dose
- After the test have half normal morning insulin dose with snack/early lunch
- Have normal evening insulin dose with evening meal
- On the day prior to the colonoscopy:
take tablets as normal at breakfast
omit all diabetes tablets after these morning doses and only restart at lunchtime or dinner after the procedure
Pre-bed take ½ (half) usual long-acting insulin dose - You should check your home glucose values every four hours
- After the procedure have a snack and return to normal tablets from lunchtime (if before midday test) or dinner onwards (if after midday test) and normal insulin dose pre-bed
Procedure is only 20 minutes, so usually no changes needed.
- Maintain your usual basal rate, and only give boluses if you need to correct for a significantly elevated reading.
- If you have any concerns about hypoglycaemia, you can use a temporary basal rate that is 80% of your usual rate.
On the day prior, continue to take GLP-1 injections as usual. Withhold morning dose on test day. If you are having a gastroscopy then you need to make sure you take only clear fluids and no solid food for 24 hours (not 6 hours) prior.
Contact our rooms or endoscopy CNC (Snr Burns) if you have:
- been admitted to hospital because of diabetes within 30 days of the procedure, or
- regular problems with hypos (low blood glucose levels)
These are guidelines only. Contact your diabetes physician, specialist diabetes nurse or GP or practice nurse for personalised advice.
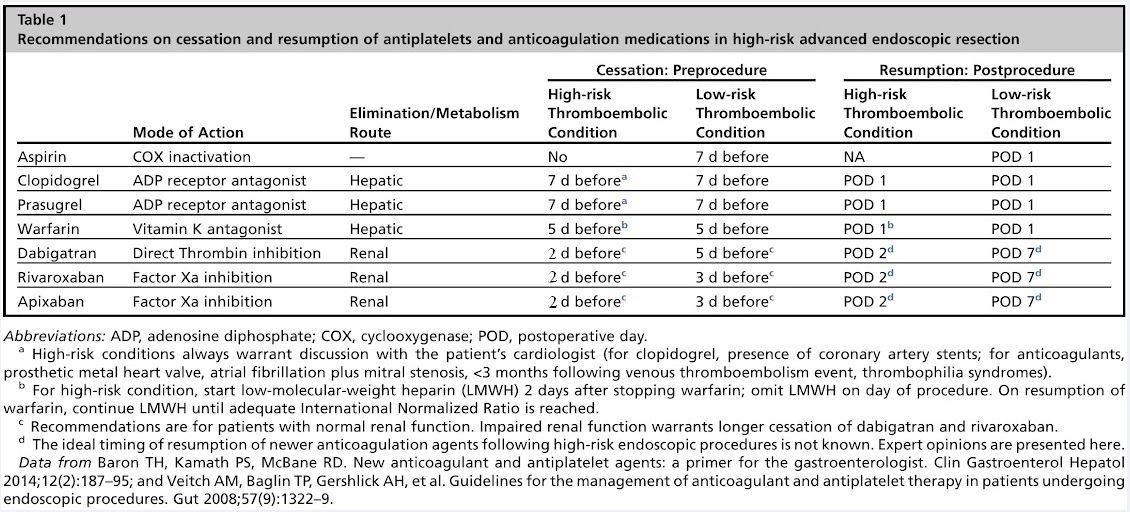
Blood thinners
Don't stop these
aspirin and NSAIDS do not need to be discontinued for endoscopic procedures.
In the absence of a bleeding disorder, they are not associated with a major increased bleeding risk including with polypectomy.
Perhaps, consider stopping NSAIDs or aspirin 5-7 days prior if used only for primary prevention.
Omit clopidogrel for 7 days and use low dose aspirin (100-150mg) monotherapy in its place (particularly if polyp removal or dilatation likely)
Reason: Decrease bleeding risk if polyps are removed. In one study 2.65% who didn't stop clopidogrel vs. 0.6% who stopped it had to come back to hospital with a bleed or need blood transfusion after polyp removal (polypectomy). Most bleeding was in patients on dual antiplatelet therapy (both aspirin and clopidogrel).
High risk for bleeding: polypectomy, PEG/PEJ placement, Balloon enteroscopy, EMR, pneumatic or bougie dilatation
Low risk for bleeding: diagnostic including mucosal biopsy, capsule or diagnostic balloon enteroscopy, argon plasma coagulation or Barrett's ablation
High risk for thrombosis (clotting): within first year of coronary stent dual antiplatelet therapy (DAPT) is important, so consider deferring elective colonoscopy and polypectomy until it is considered safe to interrupt clopidogrel therapy. For patients who cannot wait one year, the minimum duration of DAPT is 30 days and six months, for bare metal stents (BMS) and drug-eluting stents (DES) respectively.
Clopidogrel is commonly used to prevent coronary artery stent thrombosis following percutaneous coronary intervention or to prevent stroke. Discontinuation of antithrombotic therapy is the major risk factor for coronary artery stent thrombosis particularly in patients with drug-eluting stents, with events occurring as early as 5–10 days after cessation of clopidogrel therapy. Stopping clopidogrel in individuals with coronary artery disease predisposes to serious acute ischaemic events. If there is doubt, consult with cardiologist or neurologist (depending on the indication for the medication) prior to stopping it.
When to stop anticoagulant (blood thinner): for patients at low risk for thromboembolism undergoing therapeutic endoscopic procedures
- DOACs - Take last dose 3 days prior to procedure (ie. on day -3). Withhold for 3 days (with normal renal function) ie. skip day -2,-1, procedure day (eg. Monday test. Friday last dose, Skip Sat, Sun, Mon)
- dabigatran (Pradaxa 110 or 150mg bd) : skip 5 doses
- apixaban (Eliquis 5mg bd) : skip 5 doses
- rivaroxaban (
Xarelto 20mg daily) : skip 3 doses - If eGFR (CrCl) <50 mL/min then stop for 1 or 2 extra days longer as per protocol
- warfarin - Withhold for 5 days
- Withhold day -5, -4, -3, -2, -1 eg. last dose Tuesday pm (day -6) for a Monday test)
- check INR test day only if high target INR >2.5 or >=80 yo: give 1mg Vit K if INR>1.5. No need to check INR on test day if target INR<=2.5 or <80 yo
- Clexane bridging protocol
- Clexane 1mg/kg bd sci or 1.5mg/kg once daily from day -3 eg. clexane 100mg sci morning of Fri, Sat, Sun, withhold Mon test day
- Bridging with clexane only for high risk warfarin patients and if CrCl (eGFR) >30mL/min and weight <120kg
Determine and balancing bleeding and clotting risks
- stopping anticoagulation temporarily increases thromboembolic risk
- Use clexane bridging with highest risk patients: CHA2DS2-Vasc score >6; mitral mechanical valve or both prosthetic mitral and aortic valves; venous or arterial thromboembolism/CVA/TIA within three months; thrombophilia; unprovoked venous thromboembolism; and history of venous thromboembolism in patients with active cancer
- no bridging for DOACs and low risk thrombosis: bioprosthetic AVR with no CVA risk factors (HTN, AF, >75, DM, CCF), CHA2DS2-Vasc score<3, provoked thromboembolism >12 months eg. 74yo male on warfarin for AF with HTN only -CHA2DS2 = 2 - no need for bridging.
- continuing anticoagulation increases bleeding risk (HAS-BLED calculator). However, in some cases patients may prefer to take the increase bleeding risk to prevent clot or stroke risk.
When to restart anticoagulation after procedure:
Patient will be given written instructions. Usual guidelines include:
- warfarin: restart same dose on evening of (+0) or evening day after (+1)
- postop bridging only if high risk: daily clexane until INR>2.0 ( may take 5 - 10 days to attain a full anticoagulant effect )
- DOACs: restart same dose one day postop if low bleeding and day+2-7 after high bleeding risk surgery
- postop bridging with clexane 40mg if withholding for >3 days and high risk thrombosis
Special bowel preps
Optimising Bowel Preparation with Augmented/Double bowel prep: Balancing Effectiveness and Comfort
Inadequate bowel preparation increases the risk of missed pathology, but taking excessive laxatives can be uncomfortable. The goal is to find the right balance. If you have been directed here, it is to take extra bowel preparation because of a prior or high risk of inadequate bowel preparation if you took standard doses.
Recommended Augmented/Double bowel Preparation Protocol (Dr Samuel’s Standard Prep + extra doses)
What to Buy:
- Picoprep 3 (three sachets of Picoprep)
- MoviPrep (two sachets)
Preparation Timeline
7 Days Before Procedure:
- If you already take a daily laxative (e.g., Movicol 1 sachet), increase to 2 sachets daily for 7 days.
- If you do not usually take laxatives, consider Coloxyl with Senna 2 tablets at night (or Movicol 1-2 sachets daily) for 7 days.
48 Hours Before Procedure:
- Evening 7pm: Take 1L MoviPrep
- Next morning 8am: Take 1 sachet of Picoprep
Night Before the Procedure:
- 5:00 PM: Take Picoprep
- 7:00 PM: Take MoviPrep
On the Day of the Procedure:
- 4 hours before the procedure: Take the final Picoprep
- If bowel prep still seems inadequate on the test day: Take an enema 1 hour before (nursing staff will arrange)
Example Preparation Schedule (for a Monday Procedure):
- Tuesday before: Take Coloxyl with Senna 2 tablets nightly
- Saturday Night: Take 1L MoviPrep 7pm
- Sunday Morning: Take 1 sachet Picoprep 8am
- Sunday Evening:
- 5:00 PM: Picoprep
- 7:00 PM: MoviPrep
- Monday Morning (4 hours before procedure): Picoprep
- If bowel prep still seems inadequate on the test day: Take an enema 1 hour before
Timing Adjustments Based on Procedure Time
- Colonoscopy before 10 AM:
- 3:00 PM (day before): Picoprep
- 5:00 PM (day before): MoviPrep
- 7:00 PM (day before): Picoprep
- Key Rule: The most important dose is the last sachet, taken 4 hours before the procedure.
- Example: For a 10 AM appointment, take the last sachet at 6 AM.
- If the procedure is before 10 AM and the patient is an early riser (e.g., 9 AM colonoscopy), take the last sachet at 5 AM.
- If the procedure is in the afternoon and the patient wants to go out the night before, split the doses:
- 9:00 PM (night before): 1 sachet
- 6 hours before procedure: 1 sachet
- 4 hours before procedure: 1 sachet
Need to avoid Picoprep and use MoviPrep (PEG-Asc solution) only
A. 24-48 hours before test: Take a low fibre/residue diet
B. 24 hours before test: Take only clear fluids
C. Take Moviprep the night before (and in the morning only if test is after 10am)
How to prepare and take MOVIPREP
- Each Moviprep box has two sealed plastic bags
- Each plastic bag has x 1 Sachet A and x 1 Sachet B
- Pour 1 sachet A and 1 sachet B into a jug
- Make up to 1 litre with water (not chilled)
- Stir until dissolved (solution is clear or slightly hazy)
- Drink one glass (250mL) of Moviprep every 15-30 minutes, until you have drunk it all (1 litre) over approximately 1-2 hours. Take your time - there is no rush
- Drink an extra 500mL of water or clear fluids with each 1 litre of MOVIPREP taken in the next 30 mins
Follow steps 3-7 again when you due to take the second litre of Moviprep
1. Procedure time (before 10am)
The night before your procedure:
1st dose: At 7pm prepare and drink 1 litre MOVIPREP over 1-2 hour (1 cup every 15mins is recommended). Follow by 500mls (2 cups) of water in the next 30 mins. It is important to finish the full 1L of MOVIPREP. Continue clear fluids AND PREPARE YOUR SECOND DOSE OF MOVIPREP
2nd dose: At 10pm. Repeat as above.
On the day of the procedure, you can drink water but STOP 2 HOURS BEFORE procedure time (Maximum 200 mls/hr).
2. Procedure time (after 10am)
The night before your procedure:
1st dose: At 7pm the night before prepare and then drink the 1 litre MOVIPREP over 1 hour (1 cup every 15mins is recommended). Follow by 500mls (2 cups) of clear fluids in the next 30 mins. It is important to finish the full 1L of MOVIPREP.
2nd Dose: At 10 pm Make up your second dose and drink 500ml of the 2nd dose then follow by 250mls of Clear Fluids.
Continue clear fluids: Before you go to bed, put the last 500ml of MOVIPREP in the Fridge
3rd Dose: MOVIPREP:
4 hours before the procedure: Complete the rest of 500ml of the 2nd dose preparation followed by 100ml of water.You can drink water but STOP 2 HOURS BEFORE the admission time. (Maximum of 200 mls/hr).
Only to be taken with special instructions from Dr Samuel's rooms: 99% of patients with special care can tolerated standard Prepkit C
Poorly absorbed magnesium or phosphate salts taken in tablet form which act to retain water within the intestinal lumen resulting in a copious diarrhoea, thereby cleansing the bowel is one option for those who find liquid bowel preparations intolerable.
Magnesium (as sulfate monohydrate 950mg), encapsulated can be take 65 capsules (total 61.75g) so called "Colocaps" or Phosphate tablets branded as "Diacol" can be taken as 32 tablets ( 20 and then 12 split 1.105g dosed tablets). This is not for those with inflammation of the bowel or advanced renal, liver or heart disease.
Colocaps
You will need to take 65 capsules in all. The capsules are most easily swallowed 5 at a time though can be swallowed individually if preferred.
COLOCAPS (CAPSULE) MORNING PREPARATION
3.00 pm Take first 5 capsules. You should “wash down” these (and each lot of 10) capsules by drinking a large glass (at least 350ml) of clear liquid of your choice.
4.00 pm Take 10 capsules and at least 350ml drink
4.30 pm Take 10 capsules and at least 350ml drink
5.00 pm Take 10 capsules and at least 350ml drink
5.30 pm Take 10 capsules and at least 350ml drink
6.00 pm Take 10 capsules and at least 350ml drink
6.30 pm Take 10 capsules and at least 350ml drink
You should continue to drink clear fluids after completing the capsule prep
COLOCAPS (CAPSULE) AFTERNOON PREPARATION
4.30 pm Take first 5 capsules. You should “wash down” these (and each lot of 10) capsules by drinking a large glass (at least 350ml) of clear liquid of your choice.
5.00 pm Take 10 capsules and at least 350ml drink
5.30 pm Take 10 capsules and at least 350ml drink
6.00 pm Take 10 capsules and at least 350ml drink
6.30 pm Take 10 capsules and at least 350ml drink
7.00 pm Drink 1L clear fluids over 2 hours
-------------
7.00 am Take 10 capsules and at least 350ml drink
7.30 am Take 10 capsules and at least 350ml drink
8:00 pm continue to drink 1L until 2 hours before procedure
For more information: http://www.tgclinic.com.au/documents/colocaps.pdf
Diacol
You follow the stage 1 and 2 with no fibre 48 hours before and no solid food for 24 hours before. Once you start the tablet- based bowel preparation, you can only have clear fluids (a list can be found below at www.dougsamuel.com.au/colonoscopy)
1 DAY BEFORE PROCEDURE:
FIRST DOSE 6:00 PM:
One dose (Four tablets with at least 250 mls of water), every 15 minutes for a total of 5 doses (20 tablets). This should be followed by adequate glasses of water or approved clear
liquids (at least one glass per hour), in order to maintain hydration throughout your body.
LAST DOSE 6:00 AM:
One dose (Four tablets with at least 250 mls of water) every 15 minutes for a total of 3 doses (12 tablets). This should be followed by adequate glasses of water or approved clear
liquids (at least one glass per hour), in order to maintain hydration throughout your body.
DAY OF PROCEDURE:
• Drink as much clear liquid as you can before, during and after taking Diacol bowel preparation.
• Clear fluids can be taken up to four hours before your admission time. You must stop eating and drinking 4 hours before your procedure.
• Failure to adhere to this advice may result in delay or cancellation of your procedure
• Failure to follow the bowel preparation instructions can lead to poor bowel preparation and the possibility that your procedure may need to be repeated.
A successful Colonoscopy Relies on Good Preparation
Risk factors during preparation include:
• Not understanding or following the instructions.
• Drinking the wrong preparation solution, especially for
people whose diet includes a thickening agent.
• Not staying well hydrated.
• Not understanding how to use the prep solution with a
specialised diet, such as thickened liquids.
- THICKENER WARNINGS: Macrogol laxatives (Glycoprep/MoviPrep) must not be mixed with starch-based thickening agents, as macrogol opposes the thickening effect of the starch, resulting in a thin liquid which can lead to aspiration. However, macrogol laxatives can be mixed with xanthan gumbased thickening agents (such as Nestles ThickenUp). Also, people whose diet requires a thickening agent may get rarely bowel obstructions from drinking preparation solution that is overly thickened and turns to glue or an "bezoar".
Talk to the pharmacist to ensure you get a solution that’s safe and that these laxatives are the appropriate thickened IDDSI Level for the patient at the time of administration.
Thickening agents have been used to thicken macrogol laxatives, either by dissolving the macrogol in water first and then thickening, or by dissolving the macrogol powder in thickened fluid. The pharmacy can help calculate how much thickener is needed and that it is compatible.
Do not guess.
If the person uses thickening agents (such as SimplyThick or Clear DyspahgiAide), make sure they are compatible with the prepared solution and clear liquids. For the macrogol laxative, starch-based thickening agents (eg. Resource ThickenUp (starch based) - No longer available from February 2023 - different to ThickenUp Clear which is gum-based) must not be used to thicken the dose required, as the resulting mixture is thin and watery. In 2019, the Institute for Safe Medication Practices (ISMP) in Canada shared an incident where a patient who had received macrogol laxative powder mixed in a starch-based pre-thickened juice, died following suspected aspiration. The macrogol-starch mixture had resulted in a thin, watery liquid, essentially undoing the act of thickening. This interaction was also seen when macrogol powder was added to thickened apple juice, thickened water or thickened coffee, resulting in a reduction in the viscosity of the combined mixture.
Xanthan gum-based thickening agents (likely Nestle's Resource THICKENUP® Clear) can be used to thicken macrogol laxatives; it is not clear if other gum-based laxatives are suitable. Some brands of xanthan gum-based thickener are promoted
as being suitable for mixing with macrogol laxatives, and provide information on how they should be mixed, for example Swalloweze Clear and Thick & Easy Clear. Product information for starch-based thickening agents does not warn against use with macrogol laxatives.
In order to reduce the risk of inadvertently administering a thin fluid, it is good practice to visually check the consistency of all fluids before they are taken or administered
If nausea is a problem, ondansetron (Zofran) an hour before the first laxative dose and every six to eight hours during the process is effective for most people.
If you lived in a shared fridge with carers, tell everyone who lives or
works in the house where the preparation solution is located and what it’s for. Keep it separate from other drinks.
Buy clear liquids in advance. Avoid red dyes that could be confused with bleeding.
Extra tips for those with intellectual or physical impairments.
• Make sure the person is comfortable and near a bathroom. The preparation causes frequent diarrhea.
• Do not schedule appointments. Stay home.
• Offer lots of clear fluids to avoid dehydration.
• Encourage drinking all of the preparation. This may be hard
for some people to drink.
• Contact the person’s doctor about concerns, such as:
- Trouble drinking the preparation solution.
- Vomiting or nausea.
- Feeling faint, weak or ill.
- Abdominal pain that is not relieved after 10 minutes of
moving around or passing stool.
• If the person is unable to drink all of the preparation, tell the
doctor. The patient may need an enema or the colonoscopy may have to be rescheduled.